Early removal of slow-growing brain tumors dramatically improves survival
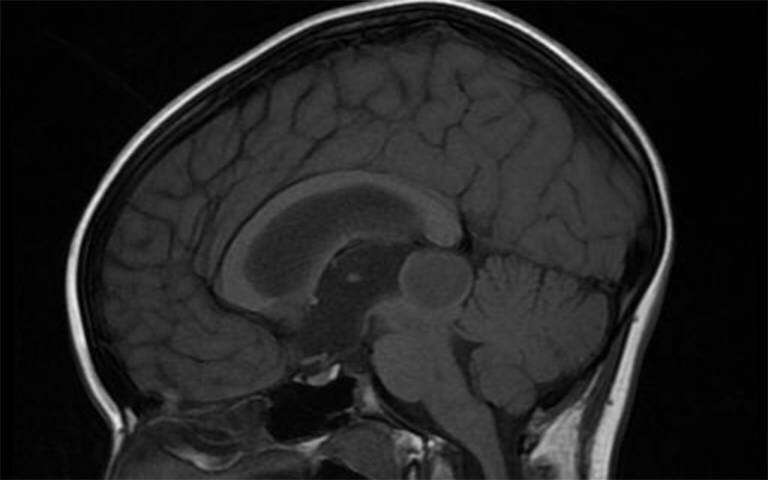
A shift in surgical practice over the last decade towards the earlier removal of a type of slow-growing but ultimately fatal brain tumor has led to dramatic improvements in survival and seizure control for patients, a study at UCLH and UCL has found.
Patients with low-grade gliomas (LGGs) had a 50 percent chance of dying within 10 years of diagnosis in 2006, compared to a 4 percent chance in 2017, according to an analysis of patient records by Dr. Jeremy Rees and his team at the National Hospital for Neurology and Neurosurgery and the UCL Queen Square Institute of Neurology, published today in Neuro-Oncology Practice.
The number of patients who were seizure-free for one year or more after surgery went up from 22 percent in 2006 to 42 percent in 2017. Under DVLA rules, these patients would be eligible to drive again, preserving their independence.
By 2017 three times as many patients were undergoing surgery to remove their tumor within one year of diagnosis compared with 2006.
Dr. Rees said: “The improvements we saw in survival and seizure control were staggering. It appears that this change in approach—to operate earlier—has led to a step change in how long patients can expect to live.
“And improvements in seizure control are vitally important for patients, due to the impacts seizures have on quality of life and driving, in particular.”
Low-grade gliomas (grades 1 and 2) make up around 30 percent of all gliomas which are the most common type of primary brain tumor. They usually progress to higher grades (3 and 4) which ultimately lead to death. LGGs have an average survival ranging from 5-15 years depending on age.
When to intervene to remove low-grade gliomas was for a long time a dilemma. Due to the risks inherent in surgery and the diffuse nature of the tumor growth, surgeons traditionally favored an approach of ‘watchful waiting’ until the tumor grew—an approach which held sway until around 2006.
Since then neuro-oncology multidisciplinary teams have taken a much more proactive approach to surgery due to a greater understanding of the risks linked to LGGs. Most patients with LGGs are now offered surgery within a year of diagnosis.
In this study, researchers at UCLH and the UCL Queen Square Institute of Neurology compared for the first time the outcomes of patients with low-grade gliomas at the same clinic 11 years apart.
Matt Solomons, a UCL medical student, analyzed records of 74 patients at Dr. Rees’s clinic at the National Hospital for Neurology and Neurosurgery in 2017 and compared them with 79 patients in the same clinic in 2006, who had been analyzed by Dr. Rimona Weil (UCLH National Hospital for Neurology and Neurosurgery and UCL Queen Square Institute of Neurology). Tumour specimens from the 2006 group were reanalyzed according to the new Brain Tumour classification by Dr. Zane Jaunmuktane, Tedani El-Hassan and Professor Sebastian Brandner in the Department of Neuropathology at UCLH/UCL, so they could be directly compared.
The two patient groups were almost identical in terms of characteristics such as age, sex, tumor location and presenting symptoms. But in the 2006 group, only 21.5 percent had early surgery, compared with 60.8 percent in the 2017 group.
Analysis showed:
- Five-year survival rates increased from 81.8 percent in 2006 to 100 percent in 2017
- 10 year survival increased from 51.7 percent in 2006 to 95.8 percent in 2017
- Rates of intractable epilepsy—where treatment fails to control a patient’s epilepsy—fell from 57 percent to 32 percent
The proportion of patients who become seizure free increased from 22 percent to 42 percent.
Importantly, numbers experiencing complications from early surgery did not go up (11.8 percent in 2006 vs 11.1 percent in 2017).
Dr. Rees said: “Given the similarities in the patient groups we saw, it is highly likely that the improvements we saw are a result of a more proactive approach to surgery.”
Source: Read Full Article


