A novel multi-epitope COVID-19 vaccine developed using reverse vaccinology
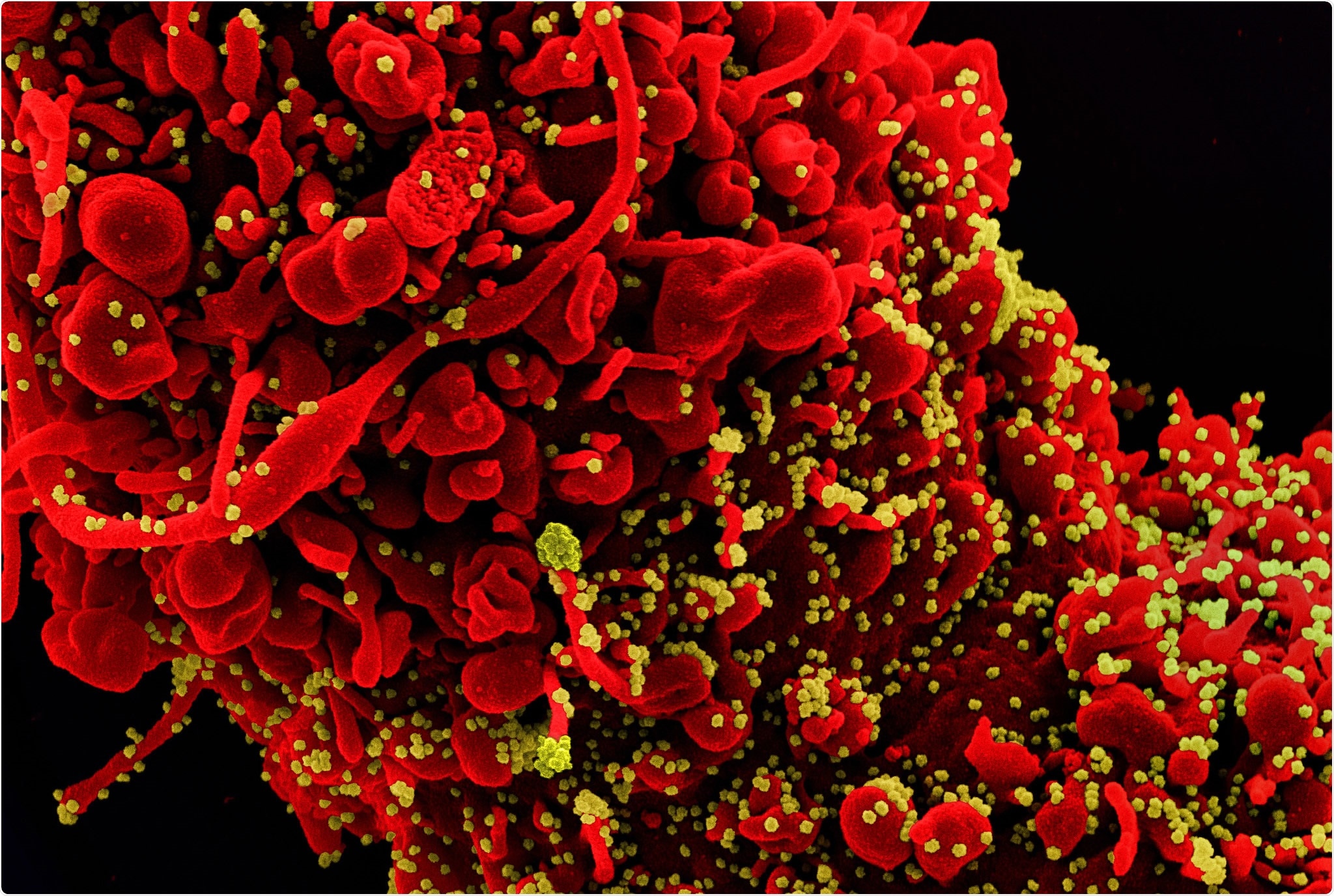
In late December 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged in Wuhan, China, and subsequently spread rapidly across the world. On the 11th of March 2020, the World Health Organization announced the global outbreak of coronavirus disease 2019 (COVID-19) as a pandemic. Scientists around the world are working extensively to develop new vaccines, therapeutics, and many other strategies to contain the pandemic.
SARS-CoV-2 is a positive-sense and single-stranded RNA virus that belongs to the genus Betacoronavirus of the Coronaviridae family. Some of the members of this family affect humans by causing common cold (HCoV-229E, HCoV-NL63, and HCoV-OC43), SARS (Severe Acute Respiratory Syndrome), and MERS (Middle East Respiratory Syndrome).
Among them, SARS-CoV-2 is the most contagious, which causes mild to severe symptoms. SARS-CoV-2 encodes both structural and non-structural proteins. The structural proteins include Spike (S) protein, Envelope (E) protein, Membrane protein (M), and Nucleocapsid protein (N).
N protein
Scientists have reported that all the structural proteins can be used as vaccine candidates. For example, N protein is associated with replicase-transcriptase complexes and is involved with the packaging, transcription, and replication of the virus. N protein stimulates potent antibodies, which in turn may trigger cytokine production.
ORF3a
Open reading frame 3a (ORF3a) is also essential for viral replication and virulence of SARS CoV. ORF3a’s function is to stimulate pro-IL-1β gene expression and IL-1β secretion that affect the lungs severely.
Researchers have revealed that very little information is available about the pathogenesis of the virus. Hence, more research, based on immunoinformatics, is required to identify the immunogenic epitopes.
Current study
A new study has been published in the Journal of Biomolecular Structure and Dynamics which focuses on the evaluation of E, M, N, ORF10, ORF8, ORF3a, and M proteins using bioinformatics tools to develop a multi-epitope COVID-19 vaccine. The researchers utilized in-silico methods to incite humoral and cellular immune responses.
Previous phylogenetic studies have revealed that SARS-CoV and SARS-CoV-2 are around 80% similar. Additionally, researchers have reported that a strong virus-specific T-cell response is essential for removing respiratory virus infections, e.g., SARS-CoV and influenza A. Also, both humoral and cellular immunity play crucial roles in protecting against these diseases.
The development of highly effective antibodies against the N protein of SARS-CoV has been observed during this infection. However, one of the major limitations of this type of antibody is that it has a shorter lifespan in convalescing patients. Along with humoral immunity, cellular responses (e.g., CD4+ and CD8+) also provide COVID-19 protection to individuals for a longer duration.
Researchers have explained that a multi-epitope vaccine could recognize and assemble B and T-cell epitopes that could efficiently trigger the immune system and elicit more potent immune responses. Recently, scientists have successfully developed vaccines using CD8+ cytolytic T-cell (CTLs), B-cell, and CD4+ helper T-cells (HTLs) epitopes.
The current study has designed a novel multi-epitope fusion protein (N protein, M protein and ORF3a) that contains antigenic epitope-rich domains.
The biological activity of this fusion protein was evaluated using bioinformatics tools. The interaction between the vaccine candidate, the innate immune system receptor (TLR4), and cellular immune system receptor (HLA-A*11:01) was assessed.
This study used the Rankpep server that analyzed HLA supertypes to predict different epitopes from N, ORF3a, and M proteins sequences according to HLA I and HLA II alleles.
For the linear epitope prediction, researchers used the Bepipred server, which also predicted epitopes of N, ORF3a, and M proteins. As both cellular and humoral responses are mandatory for effective protection against coronavirus infections, using the in-silico analysis, five epitope-rich domains that possessed high scores and shared epitopes between T and B-cell epitopes were selected.
VaxiJen v2.0 was used to determine the antigenicity of the engineered protein. The analysis of NOM protein revealed potent antigenicity without adjuvant. Further, researchers predicted the possibility of allergic reaction of the engineered protein using iAllertop and reported the absence of allergenicity in this protein.
The researchers further analyzed the physiochemical parameters (molecular weight, positive and negative charged residues, isoelectric points, etc.) and concluded that the designed protein could be a fitting vaccine candidate. They docked NOM with TLR4 (Toll-like Receptors) and HLA-A*11:01 receptors, and the interaction elicited an immune response. The molecular dynamics (MD) simulation ensured the stability of the protein structures.
Researchers of the present study used PatchDock and Firedock webservers to determine the optimal interaction between NOM protein and the immune receptors. They used global energy as the benchmark for selecting the best complexes. In a Root Mean Square Fluctuation (RMSF) analysis, values of NOM recombinant protein in MD simulations suggested fluctuation of the monomer form of the vaccine in many regions.
This indicated that the NOM recombinant protein was more stable when it was complex with the two immune receptors. Also, in a comparative study, the RMSF values of the NOM recombinant protein in complex with HLA-A*11:01 were lower than the NOM recombinant protein in complex with TLR4.
As binding energies are also lower, researchers concluded that NOM recombinant protein could bind to the HLA-A*11:01 better than the other immune receptor. This finding was also validated by a structural analysis.
- Enayatkhani, M. et al. Reverse vaccinology approach to design a novel multi-epitope vaccine candidate against COVID-19: an in-silico study. Journal of Biomolecular Structure and Dynamics. 39 (8), pp. 2857-2872, https://www.tandfonline.com/doi/full/10.1080/07391102.2020.1756411
Posted in: Medical Research News | Disease/Infection News
Tags: Antibodies, Antibody, Bioinformatics, CD4, Cell, Cold, Common Cold, Coronavirus, Coronavirus Disease COVID-19, Cytokine, Gene, Gene Expression, Immune Response, Immune System, Influenza, Lungs, Membrane, Pandemic, Protein, Receptor, Research, Respiratory, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, T-Cell, Therapeutics, Transcription, Vaccine, Virus

Written by
Dr. Priyom Bose
Priyom holds a Ph.D. in Plant Biology and Biotechnology from the University of Madras, India. She is an active researcher and an experienced science writer. Priyom has also co-authored several original research articles that have been published in reputed peer-reviewed journals. She is also an avid reader and an amateur photographer.
Source: Read Full Article