An analysis links COVID-19 to brain microvascular injury and inflammation
The ongoing COVID-19 pandemic is caused by the severe acute respiratory syndrome-2 (SARS-CoV-2), an RNA virus that belongs to the family Coronaviridae. According to research, coronavirus disease 2019 (COVID-19) patients often suffer from neurological disorders like strokes, lost taste or smell, memory loss, confusion, and delirium.
By comparing the symptoms associated with other coronavirus infections, researchers have predicted a possibility for cognitive dysfunction in COVID-19 patients.
For instance, researchers observed that during the outbreak of SARS-CoV-1 in 2002 and the Middle East respiratory syndrome (MERS) in 2012, both the viruses belonged to the family Coronaviridae and 20% of recovered patients had suffered memory impairment. Considering all the recent evidence, researchers foresee a risk of a potential surge in neurocognitive impairment such as Alzheimer's disease (AD).
Individuals with dementia such as vascular dementia, AD, or presenile dementia are more prone to be infected with SARS-CoV-2 compared to people without this ailment. Further, some of the frequent symptoms found in COVID-19 patients with dementia are hypoactive delirium, a decrease in cognitive functions, and an increased mortality rate.
Researchers have also indicated that COVID-19 infection also leads to poor neuropsychological assessments such as inattention, agitation, confusion, and disorientation.
A recent survey comprising 236,000 COVID-19 recovered individuals documents that patients who required hospitalization, ICU admission, or had encephalopathy had increased risks of neurological and psychiatric disorders. However, another study that included COVID-19 patients with mild to moderate symptoms, who did not require hospitalization, also showed mental health and neurocognitive disorders.
Some of the studies have shown that SARS-CoV-2 may infect the brain through the olfactory bulb, while others have reported that the virus is not found in the brain and cerebrospinal fluid. This virus is also reported to cause inflammation in the central nervous system (CNS) and microvascular damage. Scientists have revealed that the Spike (S) protein of SARS-CoV-2 freely crosses the blood-brain barrier (BBB) and triggers an inflammatory response in microvascular endothelial cells causing BBB dysfunction.
A new study published in the journal Alzheimer's Research & Therapy analyzed the relationship between COVID-19 infection and brain microvascular injury and neuroinflammation.
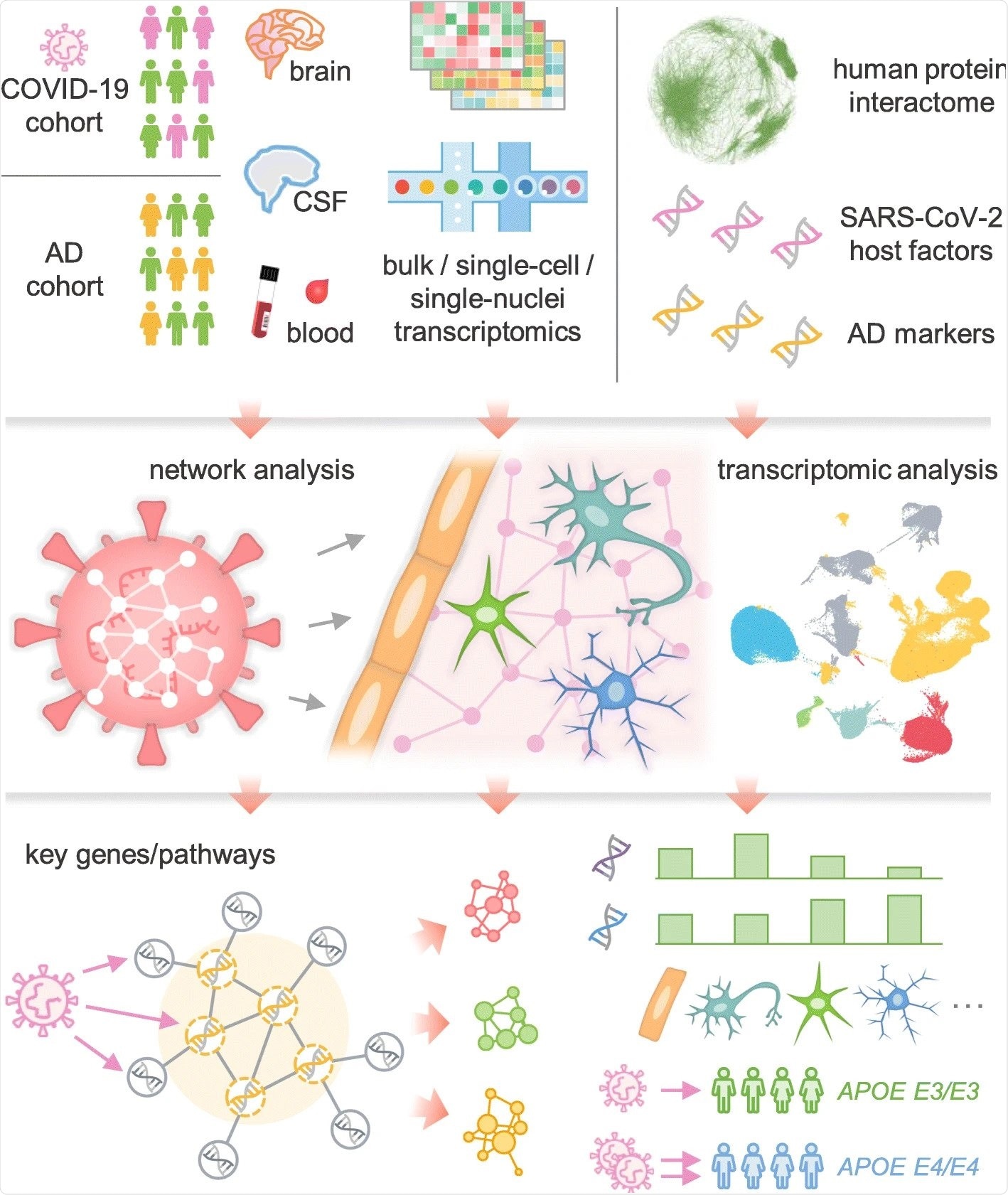
The researchers of the current study hypothesized that SARS-CoV-2 host factors would be localized in a subnetwork within the comprehensive protein-protein interaction (PPI) network and that proteins associated with certain neurologic functions would be targeted by the virus either directly or indirectly through PPIs with virus host factors. This study has revealed that limited evidence is available that associates direct brain and neuron damage with COVID-19 infection. However, a substantial body of research is available that focuses on the molecular pathways related to neuroinflammation and brain microvascular injury in COVID-19 patients.
To perform unbiased research related to pathophysiological pathways, researchers of the present study have procured multimodal omics datasets for patients with COVID-19. The data included bulk and single-cell/nucleus transcriptomic, proteomic, and interactomic PPIs. The current study has used network-based drug-disease and disease-disease proximity methods to investigate the relationship between drugs or/and drug targets and diseases. This was done to shed light on the mechanistic understandings of the pathobiology of cognitive dysfunction post-COVID-19 infection, which would, in turn, help determine novel targets for the development of effective therapeutics.
The mechanism behind the adverse effects of SARS-CoV-2 infection on the CNS, which increases the possibility of developing AD-like dementia, was studied. Researchers documented some of the gene encoding proteins associated with AD, such as RAB7A, TGFB1, and VCAM1. According to the degrees and eigenvector centralities, these proteins have shown a greater impact on the network. Additionally, based on the transcriptomic analysis profiles, these genes were found to get modified in COVID-19 patients.
In order to investigate the possibility of SARS-CoV-2 invading the brain directly, this study studied the expression of important factors that may contribute to the infection of tissues, brain regions, and brain cell types by SARS-CoV-2.
The results revealed a low expression of TMPRSS2 and ACE2 in the neurons and brains. Researchers claimed that direct invasion of SARS-CoV-2 into target neurons directly via ACE2 is highly unlikely. However, the virus can enter the brain via cerebral endothelium using receptors such as BSG and NRP. Further, a previous study supports this observation by revealing the presence of HCoVs (Human Coronaviruses) in the human brain.
Several AD marker genes such as GSTM3, TGFB1, TNFRSF1B, etc., were identified in the present research. These genes underwent modifications in COVID-19 patients. The network analysis revealed that these genes are enhanced in PPIs of immune-related gene products, such as ITGB1 and ARRB2. Further, this research has identified genes such as STAT3 and JAK1 and also found that the JAK-STAT signaling pathway is associated with inflammation in COVID-19 patients.
One of the limitations of the current study is that it considered the expression levels of the main SARS-CoV-2 entry factors and revealed low expression levels for ACE2 and TMPRSS2. However, there is a possibility that the virus may directly target the brain via unknown mechanisms. Scientists revealed that more research considering the genetic aspect and multimodal omics data from individuals with AD and infected with COVID-19 is needed, and there is room for further analysis of network-based findings.
- Zhou, Y. et al. (2021). Network medicine links SARS-CoV-2/COVID-19 infection to brain microvascular injury and neuroinflammation in dementia-like cognitive impairment. Alz Res Therapy 13, 110. https://doi.org/10.1186/s13195-021-00850-3, https://alzres.biomedcentral.com/articles/10.1186/s13195-021-00850-3
Posted in: Men's Health News | Medical Research News | Medical Condition News | Women's Health News | Disease/Infection News
Tags: ACE2, Alzheimer's Disease, Blood, Brain, Brain Cell, Cas9, Cell, Central Nervous System, Coronavirus, Coronavirus Disease COVID-19, CRISPR, Delirium, Dementia, Drugs, Encephalopathy, Gene, Genes, Genetic, Inattention, Inflammation, Interactome, Mental Health, Mortality, Nervous System, Neurological Disease, Neuron, Neurons, Pandemic, Protein, Research, Respiratory, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Signaling Pathway, Syndrome, Therapeutics, Vascular, Virus

Written by
Dr. Priyom Bose
Priyom holds a Ph.D. in Plant Biology and Biotechnology from the University of Madras, India. She is an active researcher and an experienced science writer. Priyom has also co-authored several original research articles that have been published in reputed peer-reviewed journals. She is also an avid reader and an amateur photographer.
Source: Read Full Article


