Brain cells in Alzheimer’s patients consume resources essential to neurotransmission
Alzheimer’s disease (AD), the most common type of dementia, causes the death of neurons and leads to shrinking of the brain. Patients with AD will eventually experience gradual deterioration in memory, thinking, behavior and the ability to perform everyday activities. Yet, scientists do not fully understand what causes this disease.
A recent study conducted by a team from the School of Life Sciences at The Chinese University of Hong Kong (CUHK), suggests that early changes in brain metabolism may explain the neurodegeneration. The research team is the first to discover that a special gene variant causes astrocytes of the brain to exhaust amino acids, essential for neurotransmission. The long-term insufficiency of amino acids may result in compromised neurotransmission and hence cognitive and memory impairments. Findings also indicate that direct brain supplementation of the missing amino acids was effective in alleviating the neurodegenerative outcomes as well as the functional degeneration.
These findings lay the groundwork for developing novel and targeted nutrition-centric, disease-modifying therapeutic strategies. The research paper has been published in Advanced Science.
Metabolic dysregulation is commonly observed from the prodromal stages of AD
According to the World Health Organization statistics published in 2020, around 50 million people suffer from dementia worldwide, and there are nearly 10 million new cases every year. AD is the most common form of dementia, contributing to 60 to 70 percent of cases. While the predominant approach toward AD treatments has targeted beta-amyloid, the repeated failures of clinical trials of anti-amyloid therapies highlight the pressing need to identify novel molecular targets that may underlie AD pathogenesis. Recently, a growing body of evidence has hinted that AD is a pervasive metabolic disorder in which altered cellular fuel metabolism occurs at the early prodromal stages of the disease long before the symptoms manifest. Therefore, understanding how perturbations in metabolism are related to this prodromal stage is critical to identifying targets for disease-modifying therapies.
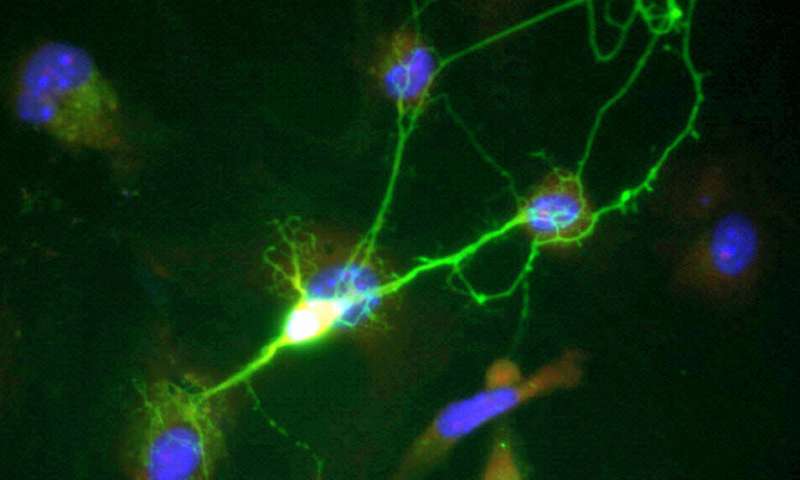
A previous study suggested an association between a synonymous single nucleotide polymorphism (SNP) in LRP6 gene and AD. In this study, the team found that this SNP is indeed correlated with diminished LRP6 gene expression in the forebrain region and the gene is predominantly expressed in astrocytes—the metabolic workhorses in the brain. By means of genetic deletion of LRP6 specifically in these cells within the adult forebrain of mice, both their cognitive and memory function were dramatically impaired. This phenotype is associated with extensive metabolic reprogramming occurring in the brain microenvironment.
Professor Kim Hei-Man Chow, principle investigator of this study and assistant professor of the School of Life Sciences, CUHK explained, “Findings show that the correct partitioning of fates of various metabolites is critical for maintaining the normal synaptic function in the brain. In normal situations, LRP6 drives a metabolic program which facilitates astrocytes to utilize glucose as its major fuel source for energy production. In the absence of LRP6 function, the entire metabolic landscape in astrocytes is rewired, rendering them unable to utilize glucose, but [instead using] glutamine, an amino acid which is also a neurotransmitter released by neurons, together with branched chain amino acids (BCAAs) as fuel. This shift in metabolic dependence not only resulted in impaired brain glycolytic capacities but also exhausted amino acids that are essential for neurotransmitter recycling and synthesis. When this situation was manifested chronically, this consequently hampered synaptic fidelity, which is the molecular basis of normal cognitive and memory functions.”
The metabolic changes affect people who harbor the gene polymorphism at LRP6 locus, and are also relevant to those with the genetic variant of the apolipoprotein E (APOE) E4 allele, the most common genetic risk factor of AD [Around 6.3 to 9.3 percent frequency in Asian (including Chinese) populations]. The research team found that protein product of the APOE-E4 allele hampers the normal functioning of LRP6 protein by trapping it inside the cell, keeping it away from the cell surface, where it carries out its functions.
Clinically ready nutrient supplementation may help manage neurodegenerative disorders
With recent advances in the field suggesting that brain metabolic dysfunction is at the core of Alzheimer’s disease, targeting the new metabolic need of the brain may become a potential strategy to manage the disease progression. The research team reports that direct brain supplementation of the missing glutamine and BCAAs was effective in alleviating the neurodegenerative outcomes, as well as the functional degeneration.
Source: Read Full Article


