Polyps and colorectal cancer risk
Patients with polyps have a higher risk of colorectal cancer, and those with sessile serrated polyps, tubulovillous adenomas, and villous adenomas had a higher colorectal cancer mortality.
Colorectal cancer is the third most common cancer and the second leading cause of cancer death worldwide. Endoscopic screening reduces colorectal cancer and mortality by detection and removal of lesions that may develop to CRC. To prevent subsequent cancer, individuals diagnosed with either conventional adenomas or sessile serrated polyps by screening endoscopy are advised to undergo colonoscopy surveillance at different intervals, depending on the most advanced findings of the index endoscopy. However, existing guidelines for colonoscopy surveillance vary widely and lack sufficient evidence
In a matched nationwide cohort study in Sweden using individual level data from the ESPRESSO study linked to nationwide health registers for the period 1993-2016, researchers from Karolinska Institutet, Harvard T.H. Chan School of Public Health, and Massachusetts General Hospital in the U.S examined the risk of colorectal cancer in patients with 178 377 different types of polyps and 864 831 matched reference individuals.
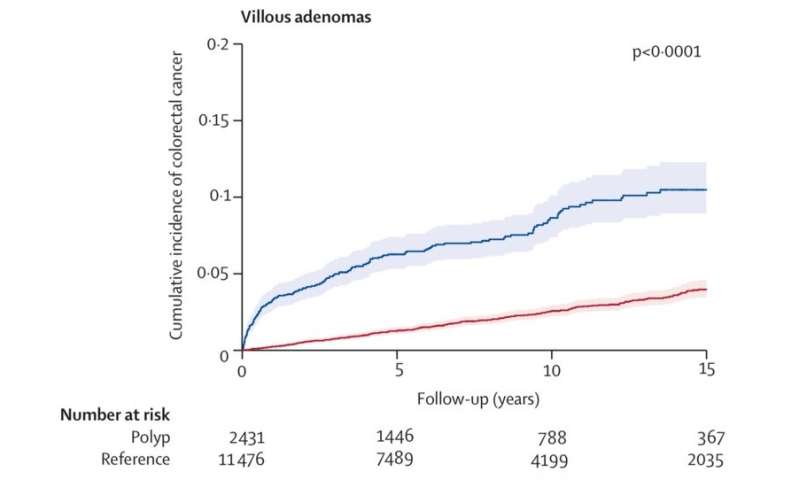
The 10-year cumulative incidence of colorectal cancer was 1.6% (95% CI 1.5–1.7) for hyperplastic polyps, 2.7% (2.5–2.9) for tubular adenomas, 2.5% (1.9–3.3) for sessile serrated polyps., 5.1% (4.8–5.4) for tubulovillous adenomas, and 8.6% (7.4–10.1) for villous adenomas compared with 2.1% (2.0–2.1) in reference individuals.
“The study provides detailed subtype-level data for the risk of colorectal cancer following polypectomy. The findings highlight the importance of close surveillance for patients with certain subtypes of polyps,” says first author and lead investigator Mingyang Song, Massachusetts General Hospital.
Compared with reference individuals, patients with any polyps had an increased risk of colorectal cancer, with multivariable HR of 1.11 (95% CI 1.02–1.22) for hyperplastic polyps, 1.77 (1.34–2.34) for sessile serrated polyps, 1.41 (1.30–1.52) for tubular adenomas, 2.56 (2.36–2.78) for tubulovillous adenomas, and 3.82 (3.07–4.76) for villous adenomas.
According to senior author and KI professor Jonas F Ludvigsson, the study suggests that follow-up of patients with different polyps could be differentiated.
Source: Read Full Article


