Catching up with omicron
Back around Thanksgiving, many families—older members newly boosted and young children freshly vaccinated—felt comfortable gathering to celebrate. Fast forward a month, and some of those winter celebrations took on a decidedly more 2020 look, owing to a new variant of SARS-CoV-2 with a name straight out of a sci-fi novel: omicron.
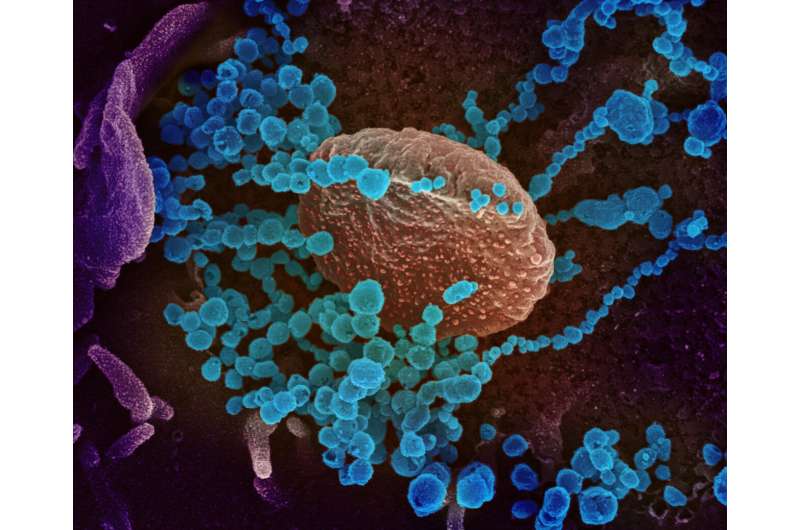
Despite being brand new to the United States—the Centers for Disease Control and Prevention announced the detection of the first case of omicron on Dec. 1—scientists are moving with lightning speed to uncover key information about the variant, including how it affects the body and why it appears to be so much more transmissible than its predecessors.
Penn Today spoke with two of those scientists working rapidly to keep up with the evolving virus, the Perelman School of Medicine’s Frederic Bushman and Susan Weiss, who co-direct the Center for Research on Coronavirus and Other Emerging Pathogens. They shared some of the scientific community’s key findings about the virus, their predictions based on decades of microbiological expertise, and their thoughts about what this new phase of the pandemic holds.
Omicron has quickly become the dominant strain in the area
Bushman’s laboratory leads the effort at Penn Medicine to sequence SARS-CoV-2 samples from clinical testing operations, hospitalized patients, and others in the Philadelphia region. Selecting samples from different groups, their testing provides a snapshot of what viral variants are circulating in the local population. His team was the first to identify the delta variant in the region last spring. Omicron showed up in the lab’s results in early December.
“We were in a delta wave,” he says, “and now we have an omicron wave coming on.”
For some samples, the lab performs whole genomic sequencing to look for particular viral mutations. Other samples are analyzed by clinical teams with PCR assays, which target and amplify select portions of the SARS-CoV-2 spike protein genome to differentiate omicron from delta. Because of the unique set of mutations in the omicron spike gene, Bushman says that certain components of the PCR tests fail to amplify their targeted genetic material. Known as a “spike drop out,” this lack of amplification can be an indication that a sample contains omicron rather than delta or another variant.
By the week leading up to Dec. 20, Bushman says 53 percent of the samples his lab tested were omicron. More recent results, he suspects, would see omicron making up an even greater proportion of samples.
A plethora of mutations are responsible for its differences
With their rapid reproduction and need to elude the immune systems of their hosts, viruses like SARS-CoV-2 are under constant pressure to evolve. A variety of mutations distinguished the “original” coronavirus, known as alpha, from subsequent variants: beta, gamma, delta, and now omicron.
When omicron was first identified in southern Africa and sequenced, scientists were surprised by the sheer number of mutations—at least 50—that set it apart from other variants. The discovery sparked concern that those changes would permit omicron to evade the hard-won immune defenses gained from vaccination and previous infection.
Exactly how omicron originated remains a mystery. While some researchers have speculated the variant arose by crossing a species barrier—going from people into an animal and back into people, accruing mutations along the way—Weiss believes the more likely explanation is less exotic.
“One theory is that it emerged in a person who was immunocompromised,” she says, “and would have had a chronic infection that might help encourage a virus to acquire immune-escape mutations.”
In this scenario, the virus would have survived in one person for weeks or even months, replicating and acquiring a variety of mutations all the while, and moving on to infect someone else.
As soon as researchers had a sequence of the omicron genome in hand, they began gaining clues as to how the virus might behave. One mutation in the gene encoding the spike protein, for example, also seen in the alpha and delta variants, makes the protein more likely to be cleaved, a process that’s required for infecting host cells and may facilitate the virus’ rapid spread. Another omicron mutation enables the spike protein to bind more strongly to host cell receptors. Additional mutations in the viral nucleocapsid protein are believed to help the virus more readily package its genome, enhancing its growth. While some changes promote viral spread, others allow it to outwit existing host immune defenses. “Both are important factors, I think” says Weiss, in explaining omicron’s newfound dominance.
Not all of omicron’s unique traits can be gleaned from analyzing its genome. Additional studies using animal models and human cells released in recent weeks by a number of groups around the world suggest that the new variant tends not to affect the lungs as severely as earlier iterations, instead robustly targeting cells in the upper respiratory system. Concentrated virus in the nose, throat, and mouth might also be a reason omicron more readily spreads from person to person, through sneezing, coughing, talking, or even just breathing.
The variant is highly transmissible and less pathogenic than previous variants
Since being detected, some good news about omicron has emerged. Thus far, while breakthrough infections are widespread, it’s clear that vaccination is still protective, slashing the risk that those immunized will experience severe disease. And overall, though highly contagious, omicron tends to cause less serious illness than earlier variants.
This shift—becoming more contagious but less harmful—does not come as a surprise to most scientists familiar with viral infections. Respiratory viruses like SARS-CoV-2 thrive when they’re moving quickly from infected host to infected host. As a result, viruses that are more transmissible have an evolutionary advantage. “These viruses are being constantly selected for a high rate of spread, high transmissibility,” Weiss says. “And this one, as we all now know, is incredibly transmissible.”
Omicron’s more mild effects go hand in hand with its increased ability to spread, Weiss says. “It’s not necessarily that the virus is evolving to be less pathogenic,” she says. “It’s more that the virus is being strongly selected for enhanced spread, with no pressure to maintain severe pathogenesis.”
The virus’s mode of transmission plays a role in the pressures that guide its evolution as well, Bushman says. To jump from person to person, a respiratory virus that is transmitted by coughs and sneezes needs its host to feel well enough to be out and about, fairly close to other people, not curled up in bed. In contrast, a disease like malaria doesn’t have that same evolutionary pressure, since “a mosquito can still bite you if you’re flat on your back,” says Bushman.
Omicron shouldn’t be overblown, or underestimated
Epidemiological models from South Africa suggest that omicron’s peak may be subsiding, and many in the U.S. fervently hope that omicron will following a similar pattern here. But this milder look for COVID-19 is not reason to do away with masks and physical distancing, the researchers say.
“I’m glad that omicron seems to be more benign,” says Bushman. “But right now, hospital admissions are absolutely soaring. We need to flatten the curve.”
Weiss concurs. “Part of me wants to just ignore it, but having so many people hospitalized is scary. It’s not the time to let down our guard.”
There’s more to COVID than omicron
While keeping attention on omicron, Weiss, Bushman, and colleagues around the University have the bigger picture in mind as well. Weiss is working to isolate the omicron variant in order to experiment with it in Penn’s Biosafety Level 3 laboratory, while continuing studies on coronaviruses more broadly. She wants to know more about how variants differ in the way they enter host cells and then affect them once they do so. Bushman, meanwhile, together with colleague Ron Collman, is continuing to look into how the microbiome influences infection and immunity in the context of COVID-19.
Penn scientists are engaged in a huge variety of other COVID-related projects, continuing to work on vaccines, antivirals, and even, in work led by the School of Veterinary Medicine, to evaluate the presence of SARS-CoV-2 in wildlife.
Source: Read Full Article


