Report: Over 60% of Saudi Arabian respondents have never taken a colorectal cancer test
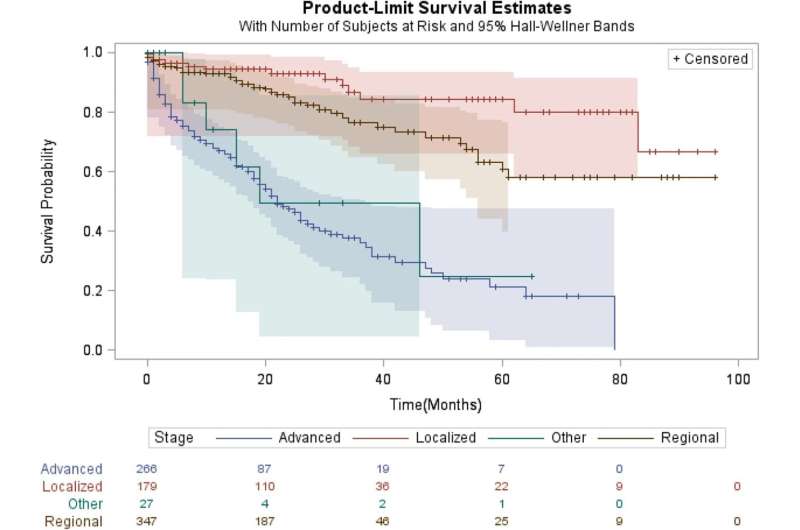
Colorectal cancer (CRC) is the most diagnosed cancer among males and third among females in Saudi Arabia, with up to two-thirds diagnosed at an advanced stage, according to the King Faisal Specialist Hospital & Research Centre.
This report shows Saudi Arabia has a high percentage of respondents (62.7%) who never took CRC tests, far higher than global average of 54.1%. This shows the Kingdom’s Early Cancer Detection Program still needs to build greater awareness among the public.
To uncover attitudes and the biggest challenges facing CRC awareness and screening, BGI Genomics released its State of Colorectal Cancer Awareness Report, marking the first-ever global survey report on the world’s third most common cancer. This report is in line with achieving Health For All, and seeks to motivate action to tackle key health challenges.
This inaugural report seeks to better understand the global state of CRC awareness, as well as attitudes and actions towards CRC screening for average risk groups and CRC screening for hereditary genetic risk groups. 1,817 respondents from six countries and regions were surveyed: the U.K (Western Europe), Hungary (Eastern Europe), Saudi Arabia (Middle East and Africa), Thailand (Southeast Asia), the Chinese mainland and Hong Kong (North Asia).
Despite 51.5% reporting that there is insufficient information about CRC and 34.5% citing costs holding them back from CRC screening, the report reveals several optimistic findings. For example, 88.8% are more willing to go for screening upon learning about the 5-year survival rate of 90% for early CRC detection.
“Early CRC detection offers the best outcome for individuals and healthcare policy. The treatment cost of late-stage CRC is sometimes more than ten times higher relative to early-stage CRC but with far lower survival rates,” said Yantao Li, Ph.D., BGI Genomics Director of Colorectal Cancer Screening Programme, South-East Asia. “That’s why more countries or regions are promoting early screening programs. For example, the European Commission is ramping up CRC screening programs.”
Other key takeaways from the report include:
Colonoscopy is the best-known screening test, but there is scope to enhance the awareness of other tests such as fecal tests. Though colonoscopy (68.2%) is the best-known screening test, it is more expensive and cumbersome relative to fecal testing which is lesser known at 49.5%. To promote this more affordable and flexible option, fecal testing awareness needs to be enhanced.
Doctors are the biggest factor for respondents to go for screening in the absence of symptoms. 62.5% will heed their doctor’s advice to undergo CRC screening. Therefore, it is vital that doctors are made more aware of CRC symptoms, ask the right questions to identify potential hereditary genetic risk and offer patients a range of screening options, to fit different lifestyles and budgets. In our opinion, the best colorectal cancer screening test is the one a patient will do.
Respondents are split when asked about bringing their family members for screening. 55.7% are aware that a family history of CRC increases their risk. According to the National Comprehensive Cancer Network (NCCN) guidelines, these family members should start screening at age 40 or 10 years before the earliest diagnosis of CRC in the family. The good news is that 67.2% who had CRC or a family history of CRC have taken their family members for screening. Conversely, only 31.2% of all respondents have taken their family members for CRC screening.
The work is published in the journal BMC Cancer.
More information:
Mesnad Alyabsi et al, Colorectal cancer survival among Ministry of National Guard-Health Affairs (MNG-HA) population 2009–2017: retrospective study, BMC Cancer (2021). DOI: 10.1186/s12885-021-08705-8
Journal information:
BMC Cancer
Source: Read Full Article


