COVID-19 human challenge study reveals detailed insights into course of infection
Findings from the UK’s world-leading human challenge study provide new insights into mild infections with SARS-CoV-2 in healthy young adults.
The collaborative study is the first in the world to perform detailed monitoring over the full course of COVID-19, from the moment a person first encounters SARS-CoV-2, throughout the infection to the point at which the virus is apparently eliminated.
The Human Challenge Programme is a partnership between Imperial College London, the Vaccine Taskforce and Department of Health and Social Care (DHSC), hVIVO (part of Open Orphan plc.), and the Royal Free London NHS Foundation Trust.
Among several key clinical insights, researchers found that symptoms start to develop very fast, on average about two days after contact with the virus. The infection first appears in the throat; infectious virus peaks about five days into infection and, at that stage, is significantly more abundant in the nose than the throat. They also found that lateral flow tests (LFTs) are a reassuringly reliable indicator of whether infectious virus is present (i.e., whether they are a likely to be able to transmit virus to other people).
The findings, published on a pre-print server and which have not yet been peer-reviewed, detail the outcomes in 36 healthy, young participants with no immunity to the virus. This landmark study, which took place at a specialist unit at the Royal Free Hospital in London, shows that experimental infection of volunteers is reproducible and resulted in no severe symptoms in healthy young adult participants, laying the groundwork for future studies to test new vaccines and medicines against COVID-19.
Professor Christopher Chiu, from the Department of Infectious Disease and the Institute of Infection at Imperial College London and Chief Investigator on the trial, said: “First and foremost, there were no severe symptoms or clinical concerns in our challenge infection model of healthy young adult participants. People in this age group are believed to be major drivers of the pandemic and these studies, which are representative of mild infection, allow detailed investigation of the factors responsible for infection and pandemic spread.
“Our study reveals some very interesting clinical insights, particularly around the short incubation period of the virus, extremely high viral shedding from the nose, as well as the utility of lateral flow tests, with potential implications for public health.”
Clinical insights
In the trial, 36 healthy male and female volunteers aged 18–30 years, unvaccinated against COVID-19 and with no prior infection with SARS-CoV-2 were given a low dose of the virus—introduced via drops up the nose—and then carefully monitored by clinical staff in a controlled environment over a two-week period. The study used virus from very early in the pandemic obtained from a hospitalized patient in the ISARIC4C study, prior to the emergence of the Alpha variant.
Eighteen of the volunteers became infected, 16 of whom went on to develop mild-to-moderate cold-like symptoms, including a stuffy or runny nose, sneezing, and a sore throat. Some experienced headaches, muscle/joint aches, tiredness and fever. None developed serious symptoms. Two participants were excluded from the final analysis after developing antibodies between initial screening and inoculation.
Thirteen infected volunteers reported temporarily losing their sense of smell (anosmia), but this returned to normal within 90 days in all but three participants—the remainder continue to show improvement after three months. There were no changes seen in their lungs, or any serious adverse events in any participant. All participants will be followed up for 12 months after leaving the clinical facility to monitor for any potential long-term effects.
Participants were exposed to the lowest possible dose of virus found to cause infection, roughly equivalent to the amount found in a single droplet of nasal fluid when participants were at their most infectious.
Accurate timeline of infection
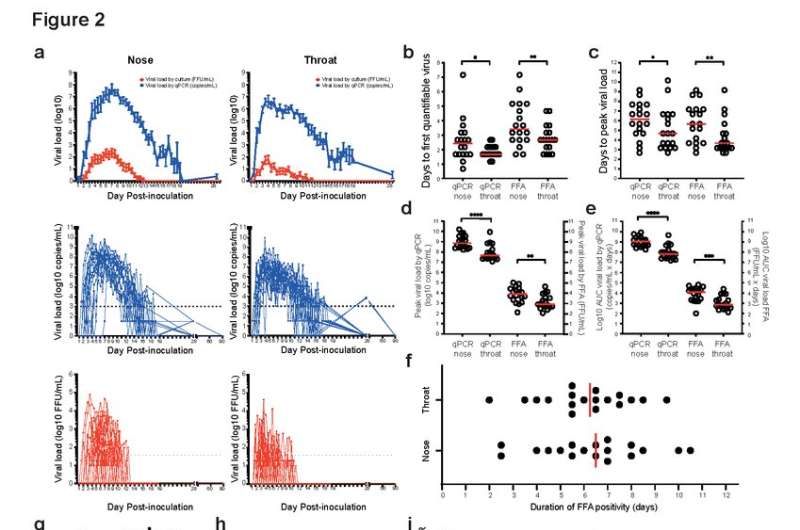
The study has also revealed some unique insights into the timeline of COVID-19, particularly during the very early period after virus exposure that cannot be looked at in other types of study, where patients are not identified until symptoms are noticed. Among the 18 infected participants, the average time from first exposure to the virus to viral detection and early symptoms (incubation period) was 42 hours, significantly shorter than existing estimates, which put the average incubation period at 5–6 days.
Following this period there was a steep rise in the amount of virus (viral load) found in swabs taken from participants’ nose or throat. These levels peaked at around five days into infection on average, but high levels of viable (infectious) virus were still picked up in lab tests up to nine days after inoculation on average, and up to a maximum of 12 days for some, supporting the isolation periods advocated in most guidelines.
There were also differences in where the most virus was found. While the virus was detected first in the throat, significantly earlier than in the nose (40 hours in the throat compared to 58 hours in the nose), levels were lower and peaked sooner in the throat. Peak levels of virus were significantly higher in the nose than in the throat, indicating a potentially greater risk of virus being shed from the nose than the mouth. This highlights the importance of proper facemask use to cover both the mouth and nose.
Lateral flow tests
Importantly, lateral flow tests (LFTs) were shown to be a good indicator of whether someone was harboring viable virus. Positive LFTs correlated well with lab-confirmed detection of virus from swabs throughout the course of infection, including in those who were asymptomatic. However, the tests were less effective in picking up lower levels of virus at the very start and end of infection.
This is the first study that has been able to provide detailed data on the early phase of infection, before and during the appearance of symptoms. While there is a possibility of missing infectious virus early in the course of infection, particularly if only the nose is tested, the researchers say these findings overall support continued use of LFTs to identify people likely to be infectious. The study provides supportive evidence that LFTs can reliably predict when someone is unlikely to infect others and can come out of isolation, and that twice-weekly rapid tests would allow diagnosis before 70–80 percent of viable virus was generated during the course of infection.
“We found that overall, lateral flow tests correlate very well with the presence of infectious virus,” said Professor Chiu. “Even though in the first day or two they may be less sensitive, if you use them correctly and repeatedly, and act on them if they read positive, this will have a major impact on interrupting viral spread.”
The authors highlight that while the model is a safe and effective approximation of real-world infection in young adults, the small sample size, reduced diversity of infected volunteers and limited follow up period may restrict the findings. However, they add that despite these limitations, the study has important implications for public health, including around proper mask-wearing, isolation periods for infectious individuals, the use of LFTs, and establishing the human challenge platform to investigate further aspects of COVID-19.
Future work will see the team determine why some people became infected and others did not and develop a challenge virus using the delta variant, which is already underway by Imperial in partnership with hVIVO and funded by the Wellcome Trust, and which could be used in follow-on trials. According to the team, with these data supporting the safety of the infection challenge model and a delta variant available, this could theoretically provide a ‘plug and play’ platform for testing new variants and therapies, including vaccines.
Professor Chiu added: “While there are differences in transmissibility due to the emergence of variants, such as delta and omicron, fundamentally, this is the same disease and the same factors will be responsible for protection against it. From the point of view of virus transmission related to the very high viral loads, we are likely if anything to be underestimating infectivity because we were using an older strain of the virus. With a newer strain, there might be differences in terms of size of response, but ultimately we expect our study to be fundamentally representative of this kind of infection.”
Professor Sir Jonathan Van-Tam, deputy chief medical officer for England, said: “Human challenge studies have been performed using other pathogens for decades, including flu and Respiratory Syncytial Virus (RSV). They need full independent ethical review and very careful planning—as has been the case this time. Every precaution is taken to minimize risk.
“Scientifically these studies offer real advantage because the timing of exposure to the virus is always known exactly, therefore things like the interval between exposure and the profile of virus shedding can be accurately described.
“This important study has provided further key data on COVID-19 and how it spreads, which is invaluable in learning more about this novel virus, so we can fine-tune our response. Challenge studies could still prove to be important in the future to speed the development of ‘next-generation’ COVID-19 vaccines and antiviral drugs.
“These data underline just how useful a tool lateral flow tests can be to pick up people when infectious and the importance of wearing a face covering in crowded, enclosed spaces.”
Dr. Andrew Catchpole, chief scientific officer at hVIVO, part of Open Orphan plc., said: “The SARS-CoV-2 characterisation study has provided invaluable insights into the progression of COVID-19 infection in healthy young adults. Importantly, the study demonstrated that SARS-CoV-2 challenge studies are safe and well tolerated by the volunteers with no serious symptoms and no Serious Adverse Events (SAEs). The study’s results have provided useful insights which could be used to inform public health decisions on COVID-19 symptoms and virus detection going forward, including isolation periods for infectious individuals, the use of LFTs, and establishing the human challenge platform to investigate further aspects of COVID-19.
“While the characterisation study was focused on the original SARS-CoV-2 strain, and there are differences in transmissibility between it and the other variants, the same factors will be responsible for protection against it, meaning the findings remain valuable for variants such as delta or omicron. These data provide a clear platform to now utilize the human challenge model to expedite product efficacy testing for new vaccines or antivirals”
Dr. Sir Michael Jacobs, consultant in infectious diseases at the Royal Free London, said: “We have vast experience of safely managing highly transmissible infections at the Royal Free Hospital and we are really pleased to have been able to play our part in this landmark study.
“The trial has already provided some fascinating new insights into SARS-CoV2 infection, but perhaps its greatest contribution is to open up a new way to study the infection and the immune responses to it in great detail and help test new vaccines and treatments.”
Source: Read Full Article


