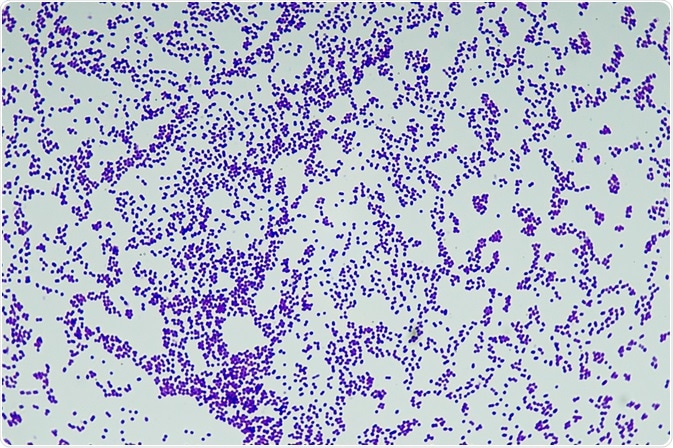
Gram Positive Bacteria
Gram positive bacteria are cells that take up a purple color in the Gram stain procedure. Their cell wall structure includes a thick peptidoglycan layer and teichoic acids.
 Credit: Katryna Kon/Shutterstock.com
Credit: Katryna Kon/Shutterstock.com
Gram staining was developed in the 1800s as a quick and simple procedure to distinguish between Gram positive and Gram negative bacteria. It is one of the first laboratory techniques taught to students of microbiology and helps classify microorganisms based on structural differences of their cell walls.
MRSA is an important example of Gram positive bacteria, characterized by its resistance to widely used antibiotics.
The Gram stain procedure
The Gram stain procedure provides a colour contrast for easy observation and helps distinguish cells into Gram positive and Gram negative bacteria. . Gram staining begins by adding a crystal violet stain to a bacterial smear and then applying iodine to form a complex that fixes the crystal violet stain within the cell.
Crystal violet is composed of positive CV ions that can penetrate the cell wall and membrane of both Gram positive and Gram negative bacteria. A decolorization step is achieved through the addition of either alcohol or acetone. Counterstaining is produced by the application of another stain such as safranin.
The different colored stains that distinguish between Gram positive and Gram negative bacteria are as a result of their different cell wall structures. Gram negative bacteria do not retain the crystal violet stain because the decolorization step disintegrates their outer membrane. The pink or red color indicating a Gram negative result is achieved by the addition of the counter stain.
Gram positive bacteria retain the crystal violet stain and a Gram positive result is indicated by a purple coloration. The counterstain does not affect the crystal violet result because it is of a lighter color.
Gram positive cell wall structure
The cell wall structure of Gram positive bacteria consists of the periplasmic space enclosed between the plasma membrane and a thick peptidoglycan layer.
In comparison to Gram negative bacteria, the periplasmic space of Gram positive bacteria is smaller in volume and the cell wall is much thicker, ranging from 15 and 80 nanometers. The thick cell wall is composed of several peptidoglycan layers, a structure based on a glycan backbone and highly cross-linked peptide chains.
Another specific characteristic of Gram positive bacteria is the presence of teichoic acids within the cell wall. Teichoic acids are anionic polyol phosphate polymers that provide rigidity to the cell wall by either anchoring to the plasma membrane or through the covalent attachment to peptidoglycan.
Anionic polymers also have similar functions to the outer membrane of Gram negative bacteria by influencing permeability, mediating interactions and acting as a scaffold for extracytoplasmic enzymes during cell-wall growth.
 Credit: Toxinmaster/Shutterstock.com
Credit: Toxinmaster/Shutterstock.com
Gram positive MRSA
Gram positive bacteria are more susceptible to treatment with antibiotics than Gram negative bacteria because they lack an outer membrane, nonetheless certain bacterial strains display antimicrobial resistance. Methicillin-resistant Staphylococcus aureus or MRSA is a common Gram positive pathogen that is resistant to all β-lactam antimicrobials including penicillin.
Many β-lactam antimicrobials are given as first line therapy for staphylococcal infection because of their superior efficacy. Resistance to these drugs means that second line agents are required, which complicate treatment regimens and negatively impact patient outcomes.
The effect of antibiotics on Gram positive bacteria is reduced because of antimicrobial resistance mechanisms such as β-lactamase production and modifications to the target site of the antibiotic. The genetic determinants of antibiotic resistance are transmitted between bacteria through both vertical and horizontal transfer, with several genes capable of being inserted in an integron leading to the resistance of multiple antimicrobials.
Therapeutic strategies for the treatment of MRSA and other antimicrobial resistant bacteria include higher antibiotic dosage, combination treatment with non-conventional drugs and the development of new drugs.
Reviewed by Gillian D’Souza, MSc
Sources:
- Beveridge, T.J. 2001. Use of the gram stain in microbiology, Biotechnic and Histochemistry, 76, pp. 111-118.
- Swoboda, J.G. et al. 2010. Wall Teichoic Acid Function, Biosynthesis, and Inhibition, ChemBioChem, 11, pp. 35-45.
- Eades, C. et al. 2017. Antimicrobial therapies for Gram-positive infections, Clinical Pharmacist, 9, e 20203363.
- Utili, R. 2001. Gram-positive bacterial infections resistant to antibiotic treatment, Annali Italiani Di Medicina Interna, 16, pp. 205-219.
Further Reading
- All Microbiology Content
- Gram Negative Bacteria
- Differentiating Between Microbial Species
- Quorum Sensing and Pseudomonas aeruginosa
- Single Cell Microbiology
Last Updated: Aug 23, 2018

Written by
Shelley Farrar Stoakes
Shelley has a Master's degree in Human Evolution from the University of Liverpool and is currently working on her Ph.D, researching comparative primate and human skeletal anatomy. She is passionate about science communication with a particular focus on reporting the latest science news and discoveries to a broad audience. Outside of her research and science writing, Shelley enjoys reading, discovering new bands in her home city and going on long dog walks.
Source: Read Full Article


