Naloxone prescriptions increased at US hospitals between 2012 and 2019, finds study
Rates of prescriptions for naloxone to people at high risk for opioid overdose, as well as co-prescribing with opioids, has increased in emergency departments throughout the United States over the past decade, providing insight on the positive impact of federal policies and regulations, according to a Rutgers study.
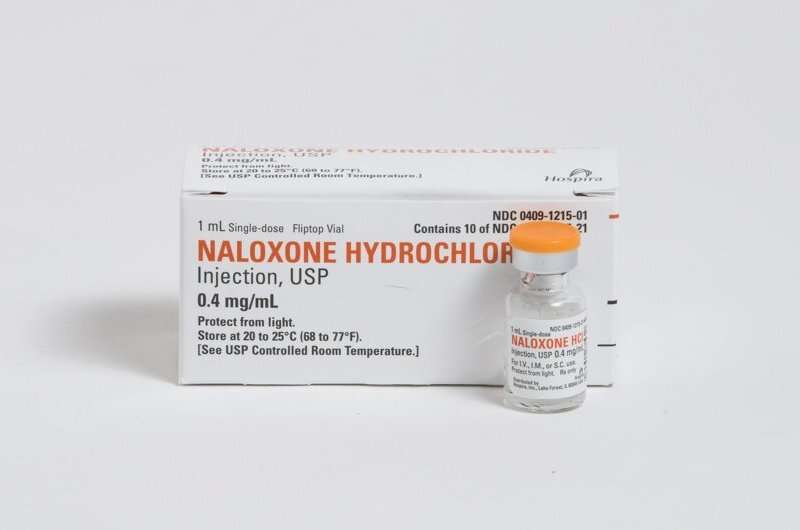
Federal opioid prescribing guidelines in 2016 made it easier for doctors to prescribe naloxone to patients at high risk for opioid overdose. When used properly, naloxone is highly effective at reversing or reducing the life-threatening adverse effects of opioids and in preventing unintentional death.
But the rise in naloxone prescriptions coincided with an increase in opioid prescriptions during emergency department (ED) stays and at discharge, researchers noted in the study, published in The American Journal of Emergency Medicine.
“It’s good to know that naloxone is being prescribed alongside opioids with increasing frequency,” said Christine Ramdin, an Instructor in the Department of Emergency Medicine at Rutgers New Jersey Medical School, and lead author of the study. “However, these prescribing rates are insufficient to account for the larger rate of patients that come to the ED with an overdose or opioid related complication. This is a trend we need to continuously improve.”
To evaluate changes in naloxone prescribing and co-prescribing with opioids in emergency departments in the U.S., Ramdin and colleagues at Georgetown University analyzed data from the National Hospital Ambulatory Medical Care Survey (NHAMCS), a nationwide representative sample conducted annually by the National Center for Health Statistics.
Of the more than 1.1 billion emergency visits recorded, an estimated 250,365 visits ended with naloxone prescribed at discharge—and the rate of naloxone prescriptions written increased over the years of the study.
There also was an increase in the rate where naloxone was prescribed at discharge when opioids were administered therapeutically during the ED visit. Although the reasons for this are unclear, it may indicate an increase in provider cognizance about the risks of opioids. At the beginning of the study period in 2012, zero visits met this criterion. At the end of the study in 2019, 22,070 visits met the criterion.
Finally, the researchers counted 44,625 visits in which opioids and naloxone were given together at discharge. No co-prescriptions were written in 2012; this climbed to 28,621 in 2019.
Although NHAMCS doesn’t monitor reasons for opioid utilization or prescribing, it does record patient intake data. The researchers found that 62 percent of patients who were prescribed naloxone at ED discharge had a substance-use disorder indicated in the record, Ramdin said.
When asked about reasons for opioid utilization during an ED visit for this population of patients, Ramdin stated, “If someone with opioid use disorder is coming in with an opioid-related complaint, they may be in withdrawal and receive an opioid for this reason in the emergency department. They could have also had a pain complaint.”
Study data was collected before the COVID-19 pandemic and additional research is needed to determine how the pandemic affected these trends, Ramdin said. While it’s likely that prescriptions continued to climb, the opposite could also be true, she said.
“The beginning of the pandemic was chaotic in emergency departments across the country, and that impacted patient care,” said Ramdin. “It’s conceivable that because of the patient load and the types of patients that providers were seeing in the ED that people with opioid-related concerns were not being prescribed naloxone at discharge. However, future research would need to be done to confirm this.”
More information:
Christine Ramdin et al, Trends in naloxone prescribed at emergency department discharge: A national analysis (2012–2019), The American Journal of Emergency Medicine (2023). DOI: 10.1016/j.ajem.2023.01.006
Journal information:
American Journal of Emergency Medicine
Source: Read Full Article


