Novel HER2 Assay to Predict HER2+ Breast Cancer Tx Response
A novel assay for measuring HER2 mRNA levels could help identify which patients with advanced HER2+ breast cancer will respond to the antibody-drug conjugate trastuzumab emtansine (T-DM1, Kadcyla) and potentially other anti-HER2 drugs, say researchers.
The HER2DX genomic assay (Reveal Genomics), recently recognized by Time magazine as one of the best inventions of 2022, incorporates 27 genes, representing four gene expression signatures, as well as tumor size and nodal status.
A recently published study that involved nearly 90 patients with advanced HER2+ breast cancer who had received T-DM1 showed that the assay could predict responses to treatment.
The findings showed that HER2-low patients, as defined using the HER2DX assay, have “an extremely poor response to T-DM1 and survival outcome,” said senior author Aleix Prat, MD, PhD, Translational Genomic and Targeted Therapies in Solid Tumors, August Pi i Sunyer Biomedical Research Institute (IDIBAPS), Barcelona, Spain.
So these patients could be spared T-DM1, which would reduce unnecessary toxicities and relatively high costs, he explained, while the HER2-high patients “might be good candidates to indicate T-DM1.”
The assay results also showed that HER2 mRNA expression was associated with a significant 30% improvement in progression-free survival (PFS) and a 25% increase in overall survival.
The study was published in the Journal of the National Cancer Institute on December 28.
Speaking to Medscape Medical News, Prat explained that the study showed that the HER2DX assay “provides three key types of information: risk of relapse, likelihood of responding to neoadjuvant systemic therapy, and precise levels of expression of the HER2 gene.
“All of this information allows patients and physicians to choose the right systemic treatment and strategy to cure the disease.”
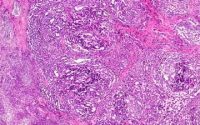
The information it provides on HER2 gene expression is also more precise than immunohistochemistry (IHC)–based assays, “both in HER2-negative and HER2-positive breast cancer.”
Prat added: “In the upcoming months, we expect to present data of our assay in HER2-negative breast cancer.”
In an accompanying editorial, Sunil Badve, MD, and Yesim Gökmen-Polar, PhD, Department of Pathology and Laboratory Medicine, Emory University, Atlanta, Georgia, welcomed the new study.
It “not only builds on the prior data regarding HER2 mRNA levels and likelihood of response but also supports the further development of the HER2DX genomic assay,” they write.
They suggest that HER2DX is likely to become the “go-to assay for assessment of risk of progression in patients with early and advanced stage HER2+ disease, and predicting the likelihood of response to neoadjuvant chemotherapy.”
Badve and Gökmen-Polar say that the “main question” that arises from the current results is, where does the HER2DX assay fit in to today’s practice?
They point out that with novel anti-HER2 agents, such as trastuzumab deruxtecan (T-DXd, Enhertu) and other antibody-drug conjugates, as well as novel tyrosine kinase inhibitors, such as tucatinib (Tukysa), the field is rapidly evolving.
“It would be interesting to see if HER2Dx could help stratify this increasingly complex landscape and provide patients and their clinicians a tool to personalize and select the most appropriate anti-HER2 agent,” they write.
“The assay could also help sequence these agents to optimize therapeutic response,” Badve and Gökmen-Polar add.
Treatment Landscape of HER2+ Breast Cancer
The authors say that the “treatment landscape” of HER2+ advanced breast cancer was changed by the introduction of T-DM1, which improved survival outcomes over those achieved with trastuzumab and a taxane and was seen as a new standard of care.
While T-DXd has since been shown to be superior to T-DM1 in the second-line setting, the authors highlight that the toxicity profile of T-DXd is “not trivial,” and there remains “uncertainty” over the best treatment sequence.
The HER2DX assay provides specific cutoffs for distinguishing HER2+ from HER2-, as well as two different levels of HER2 expression that can delineate HER2-medium and HER2-high.
The assay had already been shown to be prognostic and predictive for patients with early-stage HER2+ breast cancer, the reserachers note, so in their study, they examined whether it could be predictive of T-DM1 response in patients with advanced disease.
Their study involved 87 patients who had been diagnosed with HER2+ advanced breast cancer. These patients were treated with T-DM1 and were followed up for a median of 35.8 months. The overall response rate (ORR) was 46%, the median PFS was 5.8 months, and the median overall survival was 24.3 months.
The assay showed that expression of ERBB2 (HER2) mRNA ranged 5.1-fold between the lowest and highest quartiles. High expression was seen in 70.2% of patients, medium expression in 19.5%, and low expression in 10.3%.
High ERBB2 expression was significantly associated with ORR as a continuous variable using prespecified cutoffs, at an odds ratio of 5.29 (P = .003).
Multivariate analysis showed that among patients treated with T-DM1 in the first to third line, ERBB2 expression was significantly associated with better PFS, at a hazard ratio of 0.70 (P < .001), and overall survival, at a hazard ratio of 0.75 (P = .005).
These findings were independent of HER2 levels, as measured using IHC, hormone receptor state, age, brain metastasis, and line of therapy, the team writes.
Interestingly, both HER2DX risk and immunoglobulin signature scores were significantly associated with overall survival from diagnosis, at a hazard ratio of 1.36 (P = .04) for the former and 0.73 (P = .04) for the latter.
To further validate their findings, the team studied tumor samples from 91 patients who had been treated with trastuzumab and lapatinib in the phase 3 EGF104900 trial. In that trial, 19.8% of participants had HER2-low disease.
ERBB2 mRNA levels were associated with significantly better PFS, at a hazard ratio of 0.81 (P < .001), and overall survival, at a hazard ratio of 0.85 (P = .006), as a continuous variable and as group categories.
The study was funded by Hospital Clinic, DiSCOG – University of Padova, and Reveal Genomics. Individual authors were funded by Fundaci ón Cient í fica Asociación Española Contra el C á ncer, the European Society for Medical Oncology, and BBVA Foundation/Hospital Clinic of Barcelona. Prat has relationships with Pfizer, Lilly, Novartis, Roche, Amgen, BMS, PUMA, Nanostring Technologies, Seattle Genetics, Daiichi Sankyo, AstraZeneca, Guardant Health, Foundation Medicine, Oncolytics Biotech, and Peptomyc and patents from HER2DX. Other authors have disclosed numerous relevant financial relationships.
J Natl Cancer Inst. Published online December 28, 2022. Abstract
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article