Study reveals way to predict side-effect risk from common immune suppressant medication
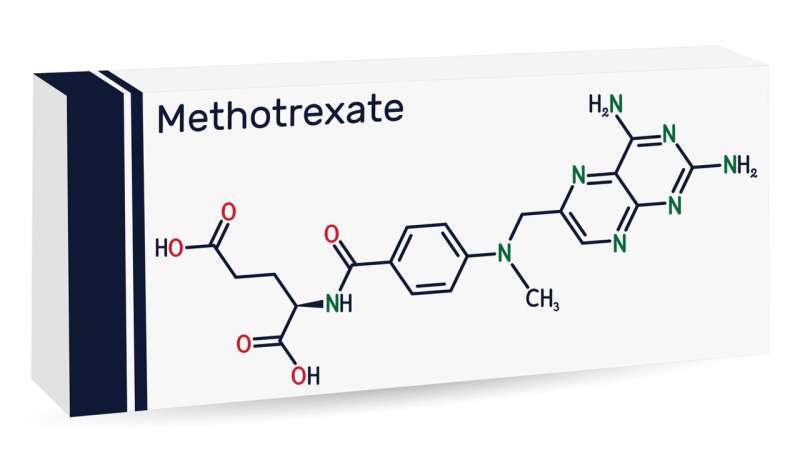
A major new study has found a method to identify people who may experience blood, kidney, or liver related side effects from methotrexate, the most commonly used immune-suppressing medicine with 1.3 million users in the UK.
The method, known as “risk stratification,” predicts the risk of abnormal blood test results during long-term methotrexate treatment using information that can be readily ascertained from electronic health records and during routine consultations.
The study, led by experts at the University of Nottingham, will have implications for people taking methotrexate. It was carried out in collaboration with colleagues from the Universities of Birmingham, Sheffield, Keele, and Nottingham University Hospitals NHS Trust.
Researchers say the method may be used by GPs and specialists to make an informed decision on how often to undertake blood-tests to screen for these side effects during long-term treatment with methotrexate, and how best to prioritize the management of their patients’ care to prevent worse outcomes. They also believe that using this method could reduce the burden of blood-testing for patients and the NHS.
Abhishek Abhishek, professor of rheumatology at the University of Nottingham led the study and said, “We are extremely pleased with the results of this study. It is the first study to develop a risk score for predicting these side effects. The method uses information available during routine consultations, at no extra cost, and provides individual risk scores that may be used alongside patient preference to decide the interval between monitoring blood-test appointments.”
“Many patients with inflammatory conditions take methotrexate for several years—often for more than ten years—and the results of this study will be useful in reducing unnecessary monitoring blood-tests for them over a long-period of time.”
“The intervals between monitoring blood tests for patients taking methotrexate is decided according to the guidelines issued by relevant specialist societies in the UK. It is imperative that the results of this study be considered by them to allow implementation of risk-stratified monitoring blood-tests. Until such recommendations are made, it is important that patients continue to attend their monitoring blood-test appointments as usual.”
“Implementing these results could vastly improve the utilization of NHS resources, save patients time and also protect the planet by reducing the carbon footprint of monitoring tests.”
Approximately 1.3 million people in the UK are prescribed methotrexate for inflammatory conditions such as rheumatoid arthritis, and skin conditions such as psoriasis. While methotrexate is effective at controlling these conditions and has become first line therapy for many illnesses, it can cause side effects such as low blood count, elevated liver enzyme, and kidney damage mostly during the first few months of treatment.
Concern about these side effects led to blood tests being performed every two to four weeks to monitor patients for these side effects during the first few months, followed by three monthly tests for everyone.
The decision to recommend blood-tests at three-monthly intervals for everyone during long-term methotrexate treatment is based on expert opinion. It is possible some patients at low risk of these side effects can undergo less frequent blood tests while others require more frequent testing.
Researchers previously reported that these side effects were infrequent after the first year of methotrexate treatment. Indeed, many abnormalities detected in the monitoring blood tests are subsequently found to be due to another illness or its treatment. Nevertheless, their detection causes anxiety, requires repeat testing, and may result in a pause in treatment that causes the condition to flare-up.
Unnecessary blood tests are a waste of patient’s time and of scarce NHS resources that can be diverted elsewhere. It is possible some people may benefit from more frequent testing while others only require six-monthly to annual testing.
The study used anonymized data from the treatment of 37,109 adults with inflammatory conditions. They had been established on methotrexate treatment in a hospital clinic and then prescribed methotrexate by their general practitioner for at least six months.
Using part of the data, researchers developed a method to predict the risk of stopping methotrexate treatment for abnormal blood count, liver enzyme level or kidney function over the next five-years and found that the method performed well in predicting these side effects in the remaining data. The method performed well across age-groups, methotrexate doses, and in different inflammatory conditions. This method involves making some calculations e.g., using an excel sheet, and can be included in GP electronic health record software for automatic calculation, ready for use during a consultation.
Professor Andrew Farmer said, “This large study using routinely collected patient data provides valuable evidence that could be used to determine whether some of the 1.3million people taking methotrexate can safely avoid unnecessary blood tests.”
“This could improve people’s lives and ease pressures on the NHS by freeing up resources for other patients who may need them more.”
“High quality research weighing up the need for tests and treatment are an important part of developing stratified medicine, to help improve future health and care practice.”
The results of the study have been published in the British Medical Journal (BMJ). A full copy of the paper, titled “Risk stratified monitoring for methotrexate toxicity in immune mediated inflammatory diseases: prognostic model development and validation using primary care data from the UK” is available.
More information:
Georgina Nakafero et al, Risk stratified monitoring for methotrexate toxicity in immune mediated inflammatory diseases: prognostic model development and validation using primary care data from the UK, BMJ (2023). DOI: 10.1136/bmj-2022-074678
Journal information:
British Medical Journal (BMJ)
Source: Read Full Article


