The hunt for a simple blood test to detect Alzheimer’s disease

Even in the prime of our lives, while still healthy and clever, our brains may be secretly developing the deadly plaques and tangles of Alzheimer’s disease. The first sign of trouble is memory loss—and, by then, damage is done.
But innovative new blood tests can now detect these hidden signs of disease, years before the onset of heartbreaking symptoms.
The tests are not yet recommended for widespread screening of the general public, because improvements are needed. But newly released data about the first FDA-approved version by C2N Diagnostics, shows that it’s 81% accurate in identifying levels of a brain protein that is a hallmark sign of Alzheimer’s disease. For the first time, the test is being used in a major National Institutes of Health-funded drug study at 75 medical centers.
“When is the best time to put out a fire? When it starts,” said Dr. Julio Rojas-Martinez of UC San Francisco’s Memory and Aging Center, which is using the test to identify people as young as 55 to participate in NIH’s AHEAD study, aimed at finding drugs to delay memory loss before symptoms begin.
Once refined and more widely available, he said, these blood tests “will be revolutionary, in that we will be able to detect who’s at risk.” While current drugs can only delay cognitive decline, not prevent it, this would enable people to enroll in research trials as early as possible.
Alzheimer’s disease, the most common form of dementia among older adults, is a brain disorder that slowly destroys memory, thinking skills and even the ability to carry out the simplest tasks. According to the Alzheimer’s Association, it afflicts 1 in 9 people over age 65.
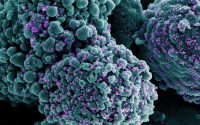
As long as two decades before symptoms, we’re accumulating toxic levels of proteins, called amyloid and tau, which form plaques and tangles.
Memory loss appears after once-healthy brain cells stop functioning, lose connections and die.
Currently, the disease is diagnosed through memory tests by a skilled neurologist, then confirmed through a costly positron emission tomography (PET) scan of the brain or an invasive spinal tap puncture to get cerebrospinal fluid. While genetic tests can help predict risk, they don’t describe the dynamic state of a brain.
“So often, people go without being identified as having Alzheimer’s or a related disorder,” said Elizabeth Edgerly, director of the Alzheimer’s Association of Northern California and Northern Nevada. “The diagnostic process can be a challenge.”
At age 58, “I definitely was having memory issues, but people just kind of dismissed it,” said Pam Montana, now 66, of Danville, a former sales executive at Intel whose agile mind could no longer memorize complex engineering concepts. Words come easily to her, but when she met with her staff, she read from notes to ensure accuracy.
“Diagnosis was really a struggle for me,” she said. “I’m chatty, and had a cute outfit on, and makeup, and they said ‘You look great.’ Everybody thinks Alzheimer’s is a grandma in a wheelchair.”
Only during a routine conversation at the doctor’s office—when she couldn’t remember where she earned her graduate degree—did alarms go off.
Her diagnosis was later confirmed by a high-tech PET scan, which involves an injection of radio-tracing fluid and lying motionless in a long tube. A diagnosis may be even harder if a patient lacks access to medical specialists and high-tech tests.
“If there was somebody that could just draw my blood and say, ‘Yeah, you have this, or you have that,’ then we could take it from there,” she said.
With so few treatments available for the debilitating condition, why might a test be useful?
“Early diagnosis is extremely helpful for several reasons,” said Lena Chow of Palo Alto, who cared for her late husband Bob Kuhar, a long-distance runner and engineer with a Ph.D. in clinical psychology. “There are lifestyle changes and numerous strategies, such as programs for ensuring socialization, to improve the quality of life. There are also pragmatic reasons, such as taking away the driver’s license, for safety.”
A major advance in Alzheimer’s research built the foundation for testing: the so-called “biomarker revolution,” which made it possible to detect plaques and tangles. A test measures the biomarkers that leak into the bloodstream.
But reliability proved elusive. Due to the blood-brain barrier, biomarkers couldn’t be found in sufficient quantities. And blood is a soup of many different substances, so traditional tools delivered inconsistent results.
Now, with the advent of better analytical techniques, even tiny amounts of these biomarkers can be detected.
“Our big leap was to detect these small molecules with very low concentrations in plasma,” said Rojas-Martinez. The new tests “are 1,000 times more sensitive. That’s what makes this enterprise possible.”
The most immediate application is for research. If patients can be identified quickly and easily, it would lower the cost of drug trials. Billions of dollars have been spent on designing treatments, with almost nothing to show for it.
“A blood test is so much more affordable, and more readily accepted,” said Edgerly.
Tests aren’t yet ready for general use. That’s because more work is needed to evaluate their performance in real-world clinical settings. And some clinicians question the prognostic value, noting that people may live with plaques in their brain and never develop symptoms.
Furthermore, analysis is technically challenging. It requires a mass spectrometer and other specialized equipment. Blood samples need rapid centrifugation and freezing, procedures that are beyond the current capabilities of most average laboratories. Collection techniques have to be standardized.
But companies are racing to create simpler, cheaper and easier tests that are fit for widespread clinical use. Some look for signs of amyloid; others, tau; still others, the ratio of the two.
The tests will continue to improve, said Rojas-Martinez. But until then, “our emphasis should be to provide care, helping the family prepare and plan for the future.”
For now, the test by C2N Diagnostics is the only one available, through an order by a physician. But at least eight other tests—by companies Quanterix, Roche, Eli Lilly, ADx, Shimadzu, MagQu, Janssen and Fujirebio—are in the pipeline.
Source: Read Full Article