What do young women in Africa want for HIV prevention? They want choice
In the first HIV prevention study to incorporate the concept of informed choice into its design, nearly all of the adolescent girls and young women who took part in the study accepted one of the two prevention products that were offered: the monthly dapivirine vaginal ring and Truvada as daily oral pre-exposure prophylaxis (PrEP). Only 2 percent turned down both. And while for the majority, the dapivirine ring was the more popular of the two—having been selected by two-thirds of the participants—most of the young women were able to use their product of choice some or most of the time.
The study, known as REACH, was conducted by the Microbicide Trials Network (MTN) at four clinical research sites in Uganda, South Africa and Zimbabwe. Results from the study’s third period, during which participants were able to choose between the dapivirine ring and daily oral PrEP after having experienced using each product, were presented today during the Conference for Retroviruses and Opportunistic Infections (CROI 2022), which is taking place virtually February 12-16.
“We know that with contraceptives, having a range of options makes it more likely of there being one that will meet an individual’s needs and preferences and that it can and will be used. Indeed, REACH is just a small example of what the potential impact could be in the realm of HIV prevention, simply by allowing young women and girls the ability to choose,” said Kenneth Ngure, Ph.D., MPH, chair of the department of community health at Jomo Kenyatta University of Agriculture & Technology in Nairobi, Kenya, and REACH protocol co-chair, who reported the study’s latest results at CROI.
Of particular relevance are the study findings suggesting that the monthly dapivirine ring could be a viable option for those adolescent girls and young women who can’t or don’t want to take daily oral PrEP.
REACH (Reversing the Epidemic in Africa with Choices in HIV prevention), or MTN-034, was a Phase IIa open-label crossover study that was designed to fill important gaps in information about the safety and acceptability of the dapivirine ring and oral PrEP, especially in girls younger than 18. REACH also sought to understand what kind of support adolescent girls and young women need to use these products as best they can, and their preferences for each. The study, which took place between February 2019 and September 2021, was funded by the U.S. National Institutes of Health.
REACH enrolled 247 participants ages 16-21 who were assigned female at birth, 86 of whom were under age 18. All participants used both Truvada as oral PrEP and the dapivirine ring, each for six months, the order of which was determined by randomization. For the final six months of the study, participants were able to choose which of the two products to use, or could decide not to use either, and could change their minds at any time.
Of the 247 participants, 227 took part in the choice period. When asked which product they wanted to use, 152 participants (67 percent) chose the ring, 71 (31 percent) chose oral PrEP and only four participants (2 percent) opted to use neither. (Thirty switched products or changed their minds at least once during the six months, although this data was not presented at CROI; a qualitative analysis looking at the reasons participants selected one product over the other, as well as why some decided to switch or chose neither is underway.)
Interestingly, those participants who chose oral PrEP over the ring were among those who had used it most regularly during the six-month period when they were assigned to that regimen.
To determine adherence, or how well participants used each product, for oral PrEP, researchers looked at the levels of drug in blood samples taken at each monthly visit., and for the ring, at the amount of residual drug left in rings participants returned after a month of use.
During the first two periods of the study, when participants used each the ring and oral PrEP, adherence to both products was higher than what had been seen in previous trials involving young women, which the researchers reported at the 11th IAS Conference on HIV Science (IAS 2021). Likewise, data reported at CROI from the study’s choice period found participants had also used the ring or PrEP some or most of the time.
Truvada as oral PrEP (or its generic equivalent, emtricitabine/tenofovir disoproxil fumarate) is approved in many countries and available to adolescent girls and young women. Although the number of young women adopting and staying on oral PrEP is lower than some would like, REACH has demonstrated that among those with a preference for oral PrEP, it’s a method that can work very well.
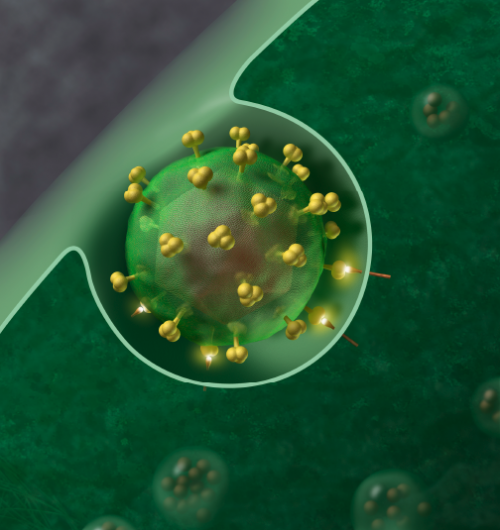
The dapivirine ring is the first biomedical HIV prevention product designed specifically for women as well as the first long-acting method. In 2020, the ring received a positive scientific opinion from the European Medicines Agency (EMA) for its use in developing countries among women at high risk for HIV who cannot or choose not to use daily oral PrEP, and in 2021, the World Health Organization (WHO) recommended the ring as an additional prevention choice for women. The ring’s developer, the nonprofit International Partnership for Microbicides (IPM), is seeking its approval in eastern and southern Africa, with approvals received in Zimbabwe and several other countries, and additional regulatory reviews underway.
Because the product’s Phase III trials were conducted among women ages 18-45, additional safety data are needed to support the ring’s use in women younger than 18. Interim results from the first two periods, also reported at IAS 2021, found both the dapivirine ring and Truvada as oral PrEP were well tolerated with no safety concerns. IPM intends to submit data from REACH, as well as from the MTN-023/IPM 030 study among adolescent girls ages 15 to 17 in the United States, to both the EMA and African regulators so that they may consider expanding the ring’s use to include adolescent girls where the product is approved.
For its part, the WHO has expressed interest in seeing what kind of insight REACH can provide for helping to better understand how best to support consistent and persistent use of both oral PrEP and the ring by adolescent girls and young women.
As part of REACH, study participants received frequent support and counseling tailored to meet individual needs and focused on helping them to use their assigned or chosen product as best they could while also ensuring they made their own decisions.
“The approaches we used seemed to work well for the young women and girls in REACH. What may be feasible or scalable at the community level and by health systems is still to be determined, and will likely depend a lot on capacity. But if there’s one thing that must be considered it’s that young women need to be allowed to make their own informed decisions about what they feel is best for them,” commented Gonasagrie (Lulu) Nair, MBChB, MPH, REACH protocol chair and senior lecturer, Centre for Medical Ethics and Law, Faculty of Medicine, at Stellenbosch University in South Africa.
“It’s not up to us to judge whether one product is better than another,” added Connie Celum, M.D., M.P.H., professor of global health and medicine and director of the International Clinical Research Center at the University of Washington in Seattle, and a REACH protocol co-chair. “Whether it’s oral PrEP, the dapivirine ring or other methods, such as injectable cabotegravir—each has its advantages and disadvantages, and what may seem to be negative for one person might actually be a plus for another.”
Globally, more than half of all people living with HIV are women, and in sub-Saharan Africa, women account for more than 60 percent of adults with HIV. HIV rates are especially high among adolescent girls and young women. According to UNAIDS, in 2020, one in four new HIV diagnoses in sub-Saharan Africa were in young women ages 15-24, despite making up only 10 percent of the population.
Source: Read Full Article


