New study identifies key gene correlated with pediatric stroke
Stroke, a devastating condition that causes damage to the brain due to interruption of blood supply, is often considered an adult disease. But children can experience strokes as well. Sadly, pediatric stroke affects one in every 4,000 newborns and an additional 2,000 older children each year.
The most common cause of stroke in children is moyamoya disease (MMD), a rare condition where the brain’s arteries progressively narrow. While this disease affects people mostly from east Asian backgrounds, especially those of Japanese descent, it develops in children from other backgrounds as well.
Dr. Adam Kundishora, MD, a sixth-year neurosurgery resident at Yale School of Medicine, recently led a team of researchers on a study that ultimately identified a genetic mutation behind some cases of MMD in people from non-Asian backgrounds—DIAPH1. They published their findings this June in the journal JAMA Neurology.
While previous research has already begun to identify susceptibility genes for moyamoya disease in Asian patients, this is one of the largest studies that have identified a gene in non-Asian patients.
“[Moyamoya] is a progressive disease of the blood vessels and we don’t really understand its pathogenesis. If we can go into the blueprints of our cells and investigate what may be wrong with the blueprint itself, we can gain insight into what pathways may be at play,” says Dr. Kundishora.
The research team used whole-exome sequencing—a powerful technique that determines the genetic code of all proteins expressed in someone’s body—to analyze the genes of 24 trios (each trio consisted of a MMD patient and their mother and father) as a discovery cohort and 84 additional trios as a validation cohort.
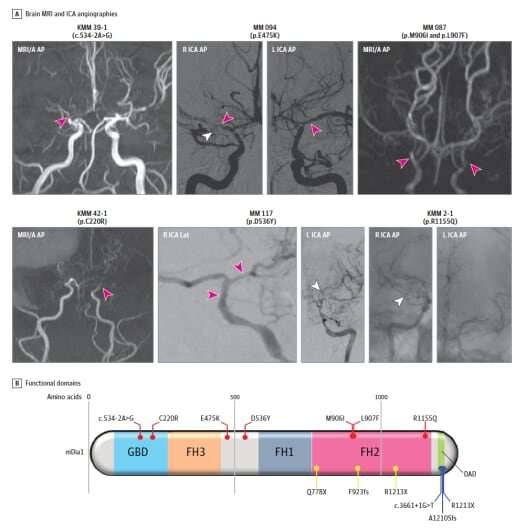
What they found was very rare—a one in one million chance, says Dr. Kundishora. Three of the 24 moyamoya patients in the discovery cohort displayed mutations of DIAPH1, a gene responsible for modulating the shape of vascular cell structures (vascular cell cytoskeletons). Three more patients of the validation cohort also showed multiple mutations of that gene.
Finding multiple mutations in the DIAPH1 gene in a small cohort size of a healthy population would be extremely unlikely. Thus, their existence in two cohorts in this study was a breakthrough moment for the team. It very strongly validated the link between DIAPH1 variations and MMD, says Dr. Kundishora.
“We hypothesize that these mutations, which interrupt DIAPH1’s central role in modulating the shape of vascular cells may lead to progressive closure of the blood vessels in the brain,” says Dr. Kundishora.
The study was a result of a collaborative, multi-center effort, with researchers including principal investigator, Dr. Kristopher Kahle, MD, Ph.D., assistant professor adjunct of neurosurgery, pediatrics and cellular & molecular physiology at Yale School of Medicine, and Dianna Milewicz, MD, Ph.D., President George H.W. Bush Chair of Cardiovascular Medicine, Director of the Division of Medical Genetics and Vice-Chair of the Department of Internal Medicine at of the University of Texas Health Science Center at Houston. (Dr. Kahle is now the director of pediatric neurosurgery at Massachusetts General Hospital).
Further research into DIAPH1 and other genes implicated in moyamoya could help doctors when they diagnose patients. Since many children present with several mini strokes (called transient ischemic attacks) before they are diagnosed with moyamoya disease, genetic testing early on could help doctors predict the patient’s prognosis and possibly prevent further strokes and brain damage.
In the future, doctors could also use this genetic information to recommend more personalized treatment approaches to MMD. For instance, given the presence of low platelets in those with DIAPH1 mutations, patients with this form of the disease may be at higher risk for bleeding. This could prompt doctors to take caution when using blood thinners, a common treatment for MMD. Eventually, researchers could even develop genetic therapies for MMD that may interrupt the progressive narrowing of blood vessels in the brain.
Dr. Kundishora and his team are now looking at animal models to understand specifically how mutations in DIAPH1 might alter biological pathways.
Source: Read Full Article


