What are the risk factors related to COVID-19-related hospitalization and mortality?
In a recent study posted to the medRxiv* preprint server, researchers assessed the risk factors associated with coronavirus disease 2019 (COVID-19)-related hospitalization or mortality.
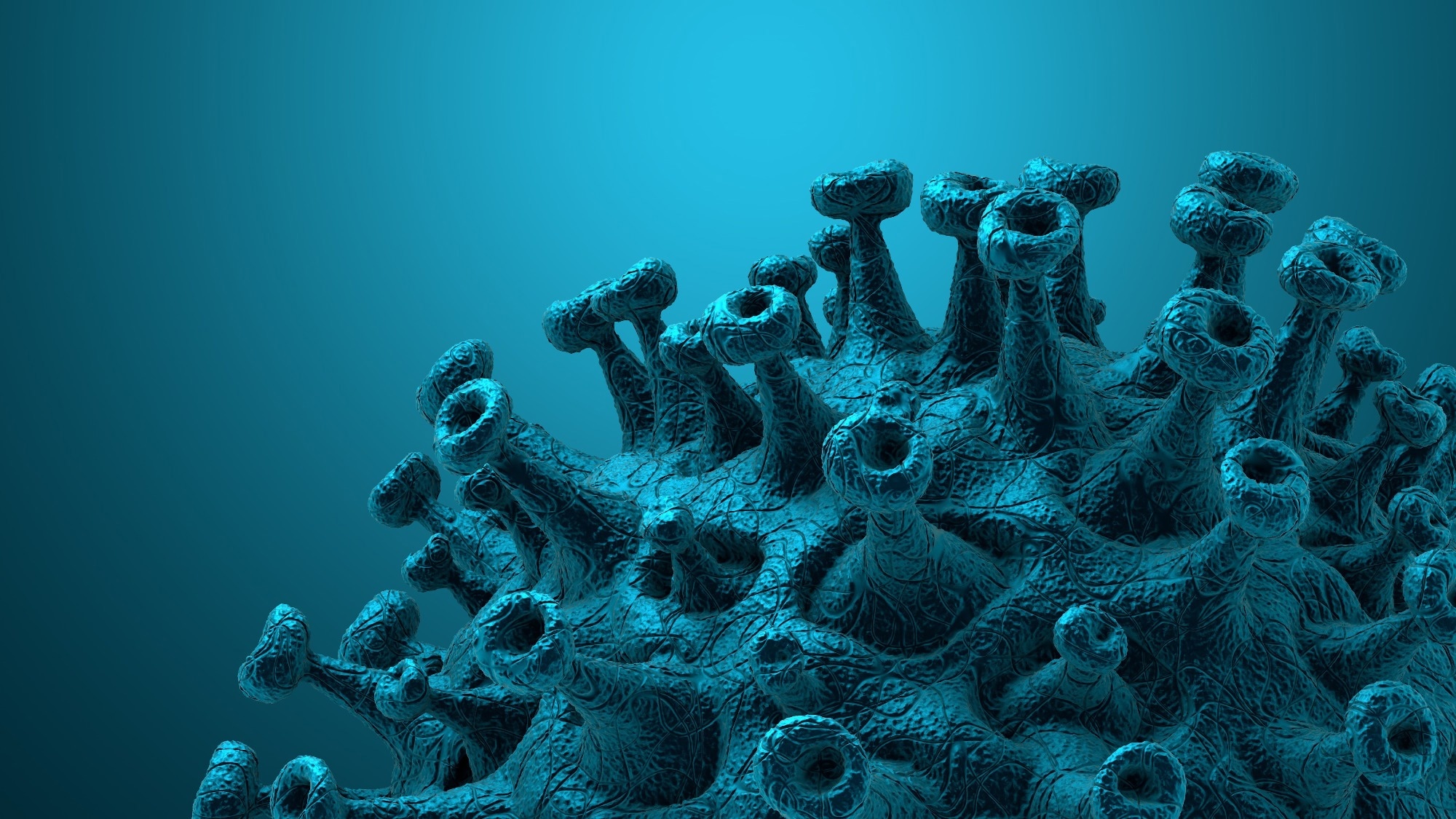
Implementing timely and efficient public health measures to curb the transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) cases and hospitalization is essential during the pandemic. Effective implementation of intervention measures is influenced by the understanding of the medical outcomes of COVID-19-infected patients and the individuals at high risk of disease severity.
About the study
In the present study, researchers examined the association of gender, age, and COVID-19 vaccination with hospitalization, admission to an intensive-care unit (ICU), or death.
The team used a case-control design including residents of Alberta, Canada, having a confirmed SARS-CoV-2 infection diagnosed in January 2022 when the SARS-CoV-2 Omicron BA.1 sublineage was dominant in the region. A transcription-polymerase chain reaction (PCR) test was employed to confirm the positive diagnosis of the individuals. Patients with severe disease outcomes such as hospitalization, admission to ICU, and/or death due to COVID-19 were categorized as cases, while those without severe disease manifestations were classified as control.
Alberta Health Care (AHS) conducted surveillance of COVID-19 cases, allocated healthcare resources, and provided clinical guidelines by utilizing data available in the Provincial Laboratory (ProvLab) database and Communicable Disease and Outbreak Management (CDOM) information system. This data was explored to detect cases and non-cases. Furthermore, data from Immunization and Adverse Reactions to Immunization (ImmARI) was utilized to assess the COVID-19 vaccination status of the participants.
The underlying conditions of the patients were also determined. A total of 24 comorbidities related to a higher risk of COVID-19 infection and/or severe disease outcomes were considered: (1) respiratory diseases including asthma, chronic obstructive pulmonary disease (COPD), and other chronic lung diseases, (2) heart diseases including heart failure, hypertension, ischemic heart disease, and other heart diseases, (3) cerebrovascular diseases including stroke and other cerebrovascular diseases, (4) metabolic diseases including diabetes type I and II, diabetes associated with an underlying condition, and other metabolic diseases, and (5) other diseases including clinically underweight, clinical obesity, liver disease, renal disease, a blood disorder, organ transplant, other immunosuppression, cancer, Alzheimer’s disease, dementia, musculoskeletal/neurological disease, and Down’s syndrome.
Each health condition was identified according to the diagnoses codes of the International Classification of Diseases (ICD)-9 and -10. Participants reporting a minimum of one visit to the physician, ambulatory visit, or admission to the hospital with applicable ICD diagnosis code noted in the past 24 months were assumed to have that medical condition. The team categorized the vaccination status of the patients into five groups: (1) unvaccinated, (2) single-dosed, (3) double-dosed with more than six months passed since the second dose, (4) double-dosed with six or fewer months passed since the second dose, and (5) vaccinated with three or more doses.
Results
The study results showed that 118,546 Alberta residents had confirmed COVID-19 infection in January 2022. Among these, 90,989 patients were included in the study sample. Among the patients assessed, 99.1% had had Omicron BA.2 infection while 0.9% had Delta infection. Almost 2% were hospitalized, 0.3% were admitted to the ICU, and 1.4% died. Furthermore, 2% of the patients displayed one or more severe disease outcomes due to COVID-19, while 98% needed neither hospitalization nor ICU admission and did not die due to the infection.
Approximately 56.5% of the patients were women, with a mean age of 42.04. Almost 72% of the patients were aged between 18 and 49 years. Additionally, 97.3% of the vaccines received by the patients were messenger ribonucleic acid (mRNA) vaccines such as BNT162b2 and mRNA-1273, and 2.2% were Vaxzevria, while 90% of the patients were double-vaccinated.
Five major underlying conditions found in the patients were hypertension, asthma, ischemic heart disease, obesity, and other metabolic diseases. Notably, 59.5% of the patients had no high-risk medical condition. Furthermore, the probability of a severe COVID-19 outcome was higher among patients who were males, in older age groups, under-vaccinated, and had more underlying conditions.
Overall, the study findings highlighted that under vaccination against COVID-19 was a major modifiable risk factor associated with severe COVID-19 disease outcome in the SARS-CoV-2 Omicron-dominant period.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- TKT Lo, Hussain Usman, Khokan C. Sikdar, David Strong, Samantha James, Jordan Ross, Lynora M. Saxinger. (2022). Risk factors for COVID-19 hospitalization or death during the first Omicron surge in adults: a large population-based case-control study. medRxiv. doi: https://doi.org/10.1101/2022.08.11.22278682 https://www.medrxiv.org/content/10.1101/2022.08.11.22278682v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Asthma, Blood, Blood Disorder, Cancer, Chronic, Chronic Obstructive Pulmonary Disease, Communicable Disease, Coronavirus, Coronavirus Disease COVID-19, covid-19, Dementia, Diabetes, Down’s Syndrome, Health Care, Healthcare, Heart, Heart Disease, Heart Failure, Hospital, Immunization, Immunosuppression, International Classification of Diseases, Ischemic Heart Disease, Laboratory, Liver, Liver Disease, Metabolic Disease, Mortality, Musculoskeletal, Neurological Disease, Obesity, Omicron, Pandemic, Polymerase, Polymerase Chain Reaction, Public Health, Renal disease, Respiratory, Ribonucleic Acid, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Stroke, Syndrome, Transcription, Transplant

Written by
Bhavana Kunkalikar
Bhavana Kunkalikar is a medical writer based in Goa, India. Her academic background is in Pharmaceutical sciences and she holds a Bachelor's degree in Pharmacy. Her educational background allowed her to foster an interest in anatomical and physiological sciences. Her college project work based on ‘The manifestations and causes of sickle cell anemia’ formed the stepping stone to a life-long fascination with human pathophysiology.
Source: Read Full Article