Study finds financial incentives for low-risk clinical trials are ethical
Use of financial incentives in two low-risk randomized clinical trials did not present ethical issues, and in one of the trials, the incentives increased study participation, according to findings published in JAMA Internal Medicine.
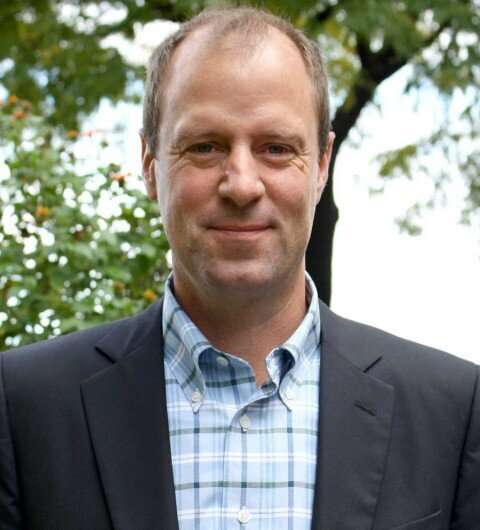
The results may help address the long-standing problem of low or insufficient enrollment in clinical trials in many areas of medicine, said Brian Hitsman, Ph.D., associate professor of preventive medicine in the Division of Behavioral Medicine, and a co-author of the study.
“Hopefully, our results will encourage people to open up to the idea of increasing enrollment in lower risk clinical trials through financial incentives to participants,” said Hitsman, who is also an associate professor of Medical Social Sciences and of Psychiatry and Behavioral Sciences.
One of the greatest barriers to accurate and efficient randomized clinical trials is the difficulty in enrolling participants. Historically, investigators have sought to increase study enrollment through several strategies, including offering financial incentives to study participants. However, whether this practice actually increases participation remained understudied.
Additionally, the ethics of the practice have long been an unanswered question, according to the authors. Two of the most common concerns among investigators with incentivizing research participation is that incentives may represent undue inducements—dismissing or downplaying the risks associated with research participation, thereby interfering with full informed consent—or unjust inducements—encouraging enrollment among people with lower income levels who otherwise would not have participated in the study.
For the current study, a total of 1,296 eligible participants were enrolled in two incentivized randomized clinical trials—one comparing smoking cessation interventions and one evaluating an ambulation (walking) intervention. Hitsman was principal investigator for the smoking trial’s clinical site at Northwestern.
Participants in the smoking trial were 50 percent women; an average age of 50 years; and 60 percent identified as Black or African American, 32.7 percent identified as white and 3.7 percent identified as multiracial. Participants in the ambulation trial were 57 percent women; an average age of 47 years; and 35 percent identified as Black or African American, 52 percent identified as white and less than one percent identified as multiracial.
Participants were then randomly assigned to receive financial incentives of either $0, $200 or $500 for participating in the smoking trial and $0, $100 or $300 for the walking trial.
The conclusion of both trials revealed that while financial incentives increased enrollment in the smoking cessation trial, they did not increase enrollment the walking trial. Noninferiority tests performed by investigators also found that incentives did not disproportionately motivate participants who reported lower income levels to enroll (unjust inducement) or a lower perceived risk of participating in the trials (undo inducement).
“One potential explanation for the different results is that the ambulation trial offered a lower risk intervention than the smoking cessation trial,” said Hitsman, who is also a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
The results suggest that while offering financial incentives for study participation are not unethical, the effectiveness and ethicality of financial incentives offered for high-risk clinical trials warrants further investigation, according to the authors.
Source: Read Full Article


