Brain studies show chronic fatigue syndrome and Gulf War illness are distinct conditions
Gulf War Illness (GWI) and chronic fatigue syndrome (CFS) share symptoms of disabling fatigue, pain, systemic hyperalgesia (tenderness), negative emotion, sleep and cognitive dysfunction that are made worse after mild exertion (postexertional malaise). Now, neuroscientists at Georgetown University Medical Center have evidence, derived from human brain studies, that GWI and CFS are two distinct disorders that affect the brain in opposing ways.
The findings, presented in two related studies at the annual meeting of the Society for Neuroscience (SFN) in Chicago, offer a new perspective on neurotoxicity and suggest that methods to effectively diagnose and treat these disorders could be developed, says the studies’ senior author, James Baraniuk, MD, a Georgetown professor of medicine.
GWI affects veterans of the 1990-1991 Persian Gulf War who were exposed to a toxic environment of nerve agents, pesticides and other neurotoxins, while the etiology of CFS is unknown. The overlapping symptoms suggest they may share some common mechanisms of disease.
Baraniuk was first to find unique physical changes in the brains of patients with GWI, and he and his colleagues have also found changes in brain chemistry between GWI and CFS. “This new work further emphasizes that chronic fatigue syndrome and Gulf War Illness are two very real, and very distinct, diseases of the brain,” he says.
The two SFN studies were led by investigators in Baraniuk’s lab. One, being presented by neuroscientist Stuart Washington, Ph.D., details how specific areas in the brain are affected by the disorders, and the second, led by student Haris Pepermintwala, MS, takes a deep dive into one of those areas, the brain stem, to illustrate the degree to which these conditions have differing effects.
Chronic fatigue syndrome/myalgic encephalomyelitis affects between 836,000 and 2.5 million Americans, according to a 2015 report by the National Academy of Medicine. Gulf War Illness developed in about one-third of the 697,000 veterans deployed to the 1990-1991 Persian Gulf War. Baraniuk says that during Operation Desert Storm, these veterans were exposed to combinations of nerve agents, pesticides and other toxic chemicals that may have triggered the chronic pain and cognitive and gastrointestinal problems.
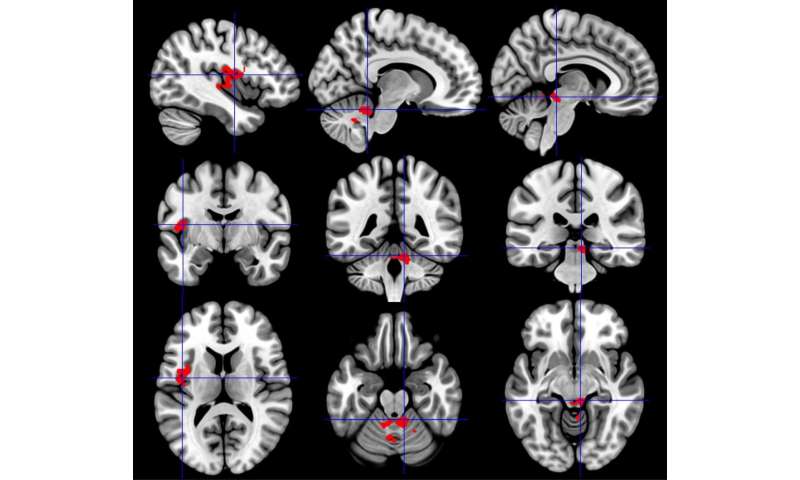
Both GWI and CFS share common features: cognitive dysfunction, pain and fatigue primarily following physical exercise. To determine how these conditions affect brain function, investigators studied neuronal activation using functional MRI (fMRI) during a cognitive task a day before and a day after bicycle exercise stress tests in their different groups: 38 CFS patients, 80 GWI patients, and a control group of 23 healthy sedentary volunteers. Brain activation during a working memory task was compared between the pre- and post-exercise fMRI studies, and between CFS and GWI groups.
Before exercise, brain activation was similar between groups. However, after exercise the CFS group showed significantly increased activation of the midbrain, while GWI had the opposite effect, with decreased activation in this vital region of the arousal network. CFS also had increased activation in the insula. In contrast, GWI, but not CFS, had a decrease in activation of the cerebellum after exercise. The findings show that specific brain regions acted in opposing ways, representing a differentiation between GWI and CFS.
While these areas are involved in pain perception, among their many other tasks, “this doesn’t mean more or less activity is directly related to pain,” says Washington. “What it does show is that the two conditions are distinct from each other and involve different cellular/molecular mechanisms.”
The second study, led by Pepermintwala, looked more closely at specific regions within the brain stem and confirmed that CFS had significantly increased activation during the cognitive task after the exercise provocations, while GWI had significantly reduced activation.
These regions are involved in vital functions for instantaneous assessments of threats, predator-prey decisions, arousal, modulation of chronic pain, sleep and other neurobehavioral functions, Pepermintwala says. But after exercise, the CFS group had significantly increased activity in the majority of regions evaluated, while the GWI patients experienced significantly decreased activation.
Source: Read Full Article


