Bernese researchers develop a second generation lung-on-chip
The lung is a complex organ whose main function is to exchange gases. It is the largest organ in the human body and plays a key role in the oxygenation of all the organs. Due to its structure, cellular composition and dynamic microenvironment, is difficult to mimic in vitro.
A specialized laboratory of the ARTORG Center for Biomedical Engineering Research, University of Bern, headed by Olivier Guenat has developed a new generation of in-vitro models called organs-on-chip for over 10 years, focusing on modeling the lung and its diseases.
After a first successful lung-on-chip system exhibiting essential features of the lung, the Organs-on-Chip (OOC) Technologies laboratory has now developed a purely biological next-generation lung-on-chip in collaboration with the Helmholtz Centre for Infection Research in Germany and the Thoracic Surgery and Pneumology Departments at Inselspital.
A fully biodegradable life-sized air-blood-barrier
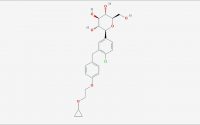
Pauline Zamprogno, who developed the new model for her PhD thesis at the OOC, summarizes its characteristics: "The new lung-on-chip reproduces an array of alveoli with in vivo like dimensions. It is based on a thin, stretchable membrane, made with molecules naturally found in the lung: collagen and elastin. The membrane is stable, can be cultured on both sides for weeks, is biodegradable and its elastic properties allow mimicking respiratory motions by mechanically stretching the cells."
By contrast to the first generation, which was also built by the team around Olivier Guenat, the developed system reproduces key aspects of the lung extracellular matrix (ECM): Its composition (cells support made of ECM proteins), its structure (array of alveoli with dimension similar to those found in vivo + fiber structure) and its properties (biodegradability, a key aspect to investigating barrier remodeling during lung diseases such as IPF or COPD). Additionally, the fabrication process is simple and less cumbersome than that of a polydimethylsiloxane stretchable porous membrane from the first-generation lung-on-chip.
Broad potential clinical applications
Cells to be cultured on the new chip for research are currently obtained from cancer patients undergoing lung resections at the Inselspital Department of Thoracic Surgery. Department Head Ralph Schmid sees a double advantage in the system: "The second generation lung-on-chip can be seeded with either healthy or diseased lung alveolar cells. This provides clinicians with both a better understanding of the lung's physiology and a predictive tool for drug screening and potentially also for precision medicine, identifying the specific therapy with the best potential of helping a particular patient."
The applications for such membranes are broad, from basic science investigations into lung functionalities and pathologies, to identifying new pathways, and to a more efficient discovery of potential new therapies."
Thomas Geiser, Head, Department of Pneumology, Inselspital and Director, Teaching and Research of the Insel Gruppe
Powerful alternative to animal models in research
As an additional plus, the new lung-on-chip can reduce the need for pneumological research based on animal models. "Many promising drug candidates successfully tested in preclinical models on rodents have failed when tested in humans due to differences between the species and in the expression of a lung disease," explains Olivier Guenat. "This is why, in the long term, we aim to reduce animal testing and provide more patient-relevant systems for drug screening with the possibility of tailoring models to specific patients (by seeding organs-on-chip with their own cells)."
The new biological lung-on-chip will be further developed by Pauline Zamprogno and her colleagues from the OOC Technologies group to mimic a lung with idiopathic pulmonary fibrosis (IPF), a chronic disease of the lung leading to progressive scarring of the lung tissue within the framework of a research project funded by the Swiss 3R Competence Center (3RCC). "My new project consists in the development of an IPF-on- chip model based on the biological membrane. So far, we have develop a healthy air-blood barrier. Now it's time to use it to investigate a real biological question," says Zamprogno.
Research group Organs-on-Chip Technologies of the ARTORG Center
This specialized group of the ARTORG Center for Biomedical Engineering Research develops organs-on-chip, focusing on the lung and its diseases, in collaboration with the Departments of Pulmonary Medicine and Thoracic Surgery of the Inselspital. The group combines engineering, in particular microfluidics and microfabrication, cell biology and tissue engineering methods, material sciences and medicine.
Their first development of a breathing lung-on-chip is further developed in collaboration with the start-up AlevoliX, with the aim to revolutionize preclinical research. Recently the group has developed an entirely biological second-generation lung-on-chip focusing on recreating the air-blood barrier of the lung. A second research direction aims at developing a functional lung microvasculature. Here, lung endothelial cells are seeded in a micro-engineered environment, where they self-assemble to build a network of perfusable and contractile microvessels of only a few tens of micrometers in diameter.
Next to pharmaceutical applications, organs-on-chip are seen as having the potential to be used in precision medicine to test the patient's own cells in order to tailor the best therapy. Furthermore, such systems have the significant potential to reduce animal testing in medical and life-science research. The OOC group operates the Organs-on-Chip Facility, providing scientists from the University of Bern, the University Hospital of Bern and beyond infrastructure and equipment to produce microfluidic devices and test organs-on-chips.
University of Bern
Zamprogno, P., et al. (2021) Second-generation lung-on-a-chip with an array of stretchable alveoli made with a biological membrane. Communications Biology. doi.org/10.1038/s42003-021-01695-0.
Posted in: Cell Biology
Tags: Blood, Breathing, Cancer, Cell, Cell Biology, Chronic, Chronic Disease, Collagen, Elastin, Fibrosis, Hospital, Idiopathic Pulmonary Fibrosis, in vitro, in vivo, Laboratory, Lung Disease, Medicine, micro, Microfluidics, Physiology, Preclinical, Pulmonary Fibrosis, Research, Research Project, Respiratory, Surgery, Tissue Engineering
Source: Read Full Article