Protein linked to heart health, disease a potential therapeutic target for dementia
By the time people with Alzheimer’s disease start exhibiting difficulty remembering and thinking, the disease has been developing in their brains for two decades or more, and their brain tissue already has sustained damage. As the disease progresses, the damage accumulates, and their symptoms worsen.
Researchers at Washington University School of Medicine in St. Louis have found that high levels of a normal protein associated with reduced heart disease also protect against Alzheimer’s-like brain damage—at least in mice. The findings, published June 21 in Neuron, suggest that raising levels of the protein—known as low-density lipoprotein receptor (LDL receptor)—could potentially be a way to slow or stop cognitive decline.
The discovery of LDL receptor as a potential therapeutic target for dementia is surprising since the protein is much better known for its role in cholesterol metabolism. Statins and PCSK9 inhibitors, two groups of drugs widely prescribed for cardiovascular disease, work in part by increasing levels of LDL receptor in the liver and some other tissues. It is not known whether they affect LDL receptor levels in the brain.
“There are not yet clearly effective therapies to preserve cognitive function in people with Alzheimer’s disease,” said senior author David Holtzman, MD, the Andrew B. and Gretchen P. Jones Professor and head of the Department of Neurology. “We found that increasing LDL receptor in the brain strongly decreases neurodegeneration and protects against brain injury in mice. If you could increase LDL receptor in the brain with a small molecule or other approach, it could be a very attractive treatment strategy.”
The key to the importance of LDL receptor lies in a different protein, APOE, that also is linked to both cholesterol metabolism and Alzheimer’s disease. High cholesterol in the blood is associated with increased risk of Alzheimer’s disease, although the exact nature of the association is unclear.
During the long, slow development of Alzheimer’s disease, plaques of a protein called amyloid gradually accumulate in the brain. After many years, another brain protein called tau starts forming tangles that become detectable just before Alzheimer’s symptoms arise. The tangles are thought to be toxic to neurons, and their spread through the brain foretells the death of brain tissue and cognitive decline. First author Yang Shi, Ph.D., a postdoctoral researcher, and Holtzman previously showed that APOE drives tau-mediated degeneration in the brain by activating microglia, the brain’s cellular janitorial crew. Once activated, microglia can injure neural tissue in their zeal to clean up molecular debris.
Higher levels of LDL receptor limit the damage APOE can do in part by binding to APOE and degrading it. Higher levels of LDL receptor in the brain, therefore, should pull more APOE out of the fluid surrounding brain cells and mitigate damage even further, the researchers reasoned.
As part of this study, Shi, Holtzman and colleagues including co-senior author Jason Ulrich, Ph.D., an associate professor of neurology, studied mice predisposed to develop Alzheimer’s-like neurodegeneration because they had been genetically modified to develop tau buildup in the brain, much like people with Alzheimer’s disease and other forms of dementia. The researchers bred the tau mice with mice genetically modified to express high levels of LDL receptor in their brains. The resulting offspring had high levels of LDL receptor and a propensity to develop Alzheimer’s-like brain damage by the time they were 9 months old, which is similar to middle age in a person.
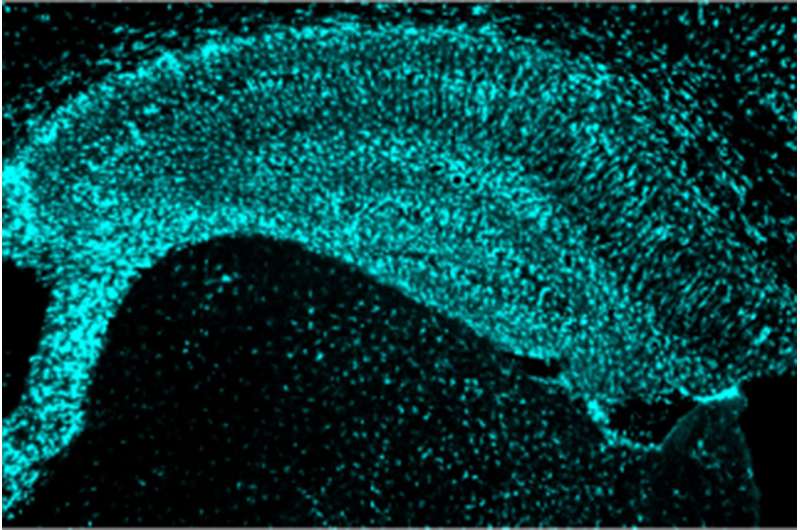
Then, the researchers compared the four groups: normal mice, tau mice, mice with high levels of LDL receptor, and tau mice with high levels of LDL receptor. At 9 months, the normal mice and the mice with high levels of LDL receptor had healthy looking brains. The tau mice had severe brain atrophy and neurological damage. In comparison, the tau mice with high levels of LDL receptor were in much better shape. They had significantly less brain shrinkage and damage, their levels of certain forms of tau and APOE were significantly lower, and their microglia were shifted toward a less damaging pattern of activation.
Source: Read Full Article


