Defining the Parkinson’s microbiome strengthens links to gut health
Researchers from the Quadram Institute have carried out a meta-analysis of the gut microbiome in Parkinson’s disease, giving the clearest picture to date of the changes associated with the condition.
By re-analyzing data from ten different studies, a common pattern of changes in the abundance of bacteria types in Parkinson’s disease emerges, suggesting that the alteration in the gut microbiome might trigger some of the gastrointestinal problems seen in patients.
Parkinson’s is a progressive condition that affects nerve cells that produce dopamine, which coordinates movement. As more nerve cells die, less dopamine is produced, leading to gradually worsening tremors, slower movement and muscle stiffness.
In addition, many people with Parkinson’s disease have gastrointestinal problems that can show several years before the physical movement symptoms. They may also have inflammation and “leaky” gut, signs of an imbalanced gut microbiome.
These observations have prompted genome sequencing studies to identify the types of bacteria in the microbiome of people with Parkinson’s disease, and compare that with people without the condition.
Several studies have shown differences in the Parkinson’s microbiome, but no clear consensus has emerged. Differences across studies may reflect different methodologies, but also the inherent variability in the human microbiome, shaped by lifestyle and dietary variations in different populations around the world. Drug treatment regimens and antibiotic usage also impact on gut bacteria, so variability between different studies isn’t a surprise, but it does make drawing definitive conclusions on the association between the microbiome and Parkinson’s harder.
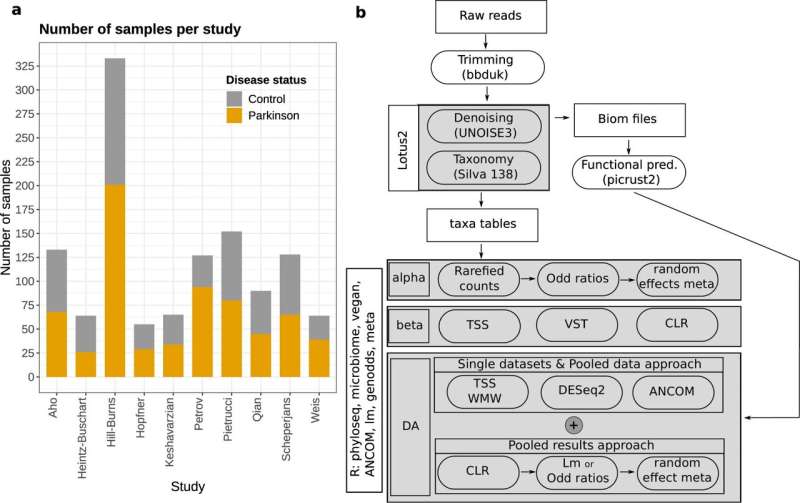
To address this, the Quadram Institute researchers sought to reanalyse the patient data paired with their control collected across studies from six different countries. This large pool of 1200 samples allowed the researches to identify robust differences between the microbiomes of people with or without Parkinson’s disease. The study was supported by the Biotechnology and Biological Sciences Research Council (BBSRC), part of UKRI.
The meta-analysis, published in the journal npj Parkinson’s Disease, confirmed that the Parkinson’s microbiome is different with a reduction in the dominant bacteria usually found in a healthy human gut.
But to understand how changes in the microbiome affect health, we need to know what those bacteria are doing. What chemicals, metabolites or signals do they produce and how does this change with the disease?
The researchers report that some of the depleted bacteria in Parkinson’s produce butyrate, which is used by the cells that line the gut to maintain its integrity as a barrier. Butyrate and other short chain fatty acids also play important roles in interactions between the gut, the nervous system and the brain.
In previous studies, Parkinson’s disease patients were shown to have lower butyrate levels and increased gut lining inflammation and permeability. Similar depletions in key bacterial species, butyrate levels and gut lining integrity are seen in patients with Inflammatory Bowel Disease (IBD) and IBD patients have a 20%-30% higher risk of developing Parkinson’s disease.
Other bacteria involved in methane production are enriched in the gut of Parkinson’s patients. This together with an increased abundance of bacteria able to degrade the mucus within the gut might affect transit time and explain the constipation problems that are recurrently observed in Parkinson’s patients.
This study backs up and adds to the evidence linking the gut microbiome, gut inflammation and immune function in Parkinson’s, and provides intriguing hints into potential mechanisms by which the gut microbiome influences the disease.
However, the team underlines that the available data can’t answer the question of whether the microbiome alterations cause Parkinson’s Disease or are an effect of it, and suggest sampling strategies that could help understand the causal link between the disease and the gut microbiome.
Dr. Stefano Romano who led the study commented “The variability across studies is very big. However, we can still detect differences between the gut microbiome of patients and controls. This means that microbiome alterations in Parkinson’s disease are consistent across sampling cohorts.”
“There is a clear need to further research gut microbial changes linked to diseases in diagnostic or prognostic applications.”
Microbiome alterations may also be used as biomarkers, especially useful for spotting the earliest onset of the disease, and open new targets for therapies.
Source: Read Full Article


