New research supports clinical utility of circulating tumor cell count for metastatic breast cancer
Menarini Silicon Biosystems has announced the publication of a research study providing support for the reliability of using circulating tumor cell (CTC) count to guide frontline therapy choice for patients with estrogen receptor-positive (ER+), HER2-negative (HER2) metastatic breast cancer. Published in the November issue of JAMA Oncology, this is the first study to support clinical utility of CTC count in a randomized clinical trial.
“Based on our research, the use of the CTC count represents the first objective and reproducible decision tool to help physicians choose between hormone therapy or chemotherapy for this particular group of patients,” said lead author Francois-Clement Bidard, MD, Ph.D., Professor of Medical Oncology at Institut Curie and University of Versailles. “Furthermore, our results indicate that the CTC count complements but does not duplicate the physician’s opinion on which treatment to choose and should be included in the decision algorithm. This CTC test may help customizing treatment decisions for all women suffering from ER+ HER2- metastatic breast cancer.”
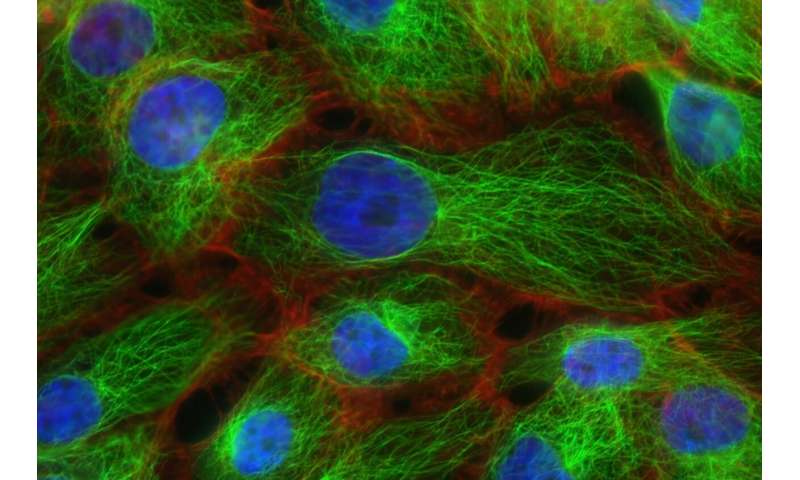
The randomized Phase III trial, known as the STIC CTC study, included 778 women with Stage 4 ER+, HER2- breast cancer and compared the outcomes of treatment decisions based on physician assessment vs. CTC count. Half of the patients were randomly assigned to the clinically driven treatment group, where treatment was selected by a physician based on clinical factors. The other half were assigned to a CTC-driven treatment group, in which patients with 5 or more CTCs in 7.5 mL of blood received chemotherapy, and those with less than 5 CTCs in 7.5 mL received hormone therapy. Menarini Silicon Biosystems’ CELLSEARCH CTC System was used to capture and isolate tumor cells circulating in the blood in all patients.
The results supported the reliability and clinical utility of using the CTC count to guide front line therapy choice. For most patients in the clinically driven arm, the CTC count correlated with the physician’s choice of treatment. In the CTC-driven group, escalation of treatment to frontline chemotherapy for patients with high CTC count significantly improved progression free survival (PFS), while de-escalation to hormone therapy for patients with low CTC count did not have a detrimental impact on PFS or overall survival (OS).
“The results of the STIC CTC study provide evidence that the CTC count can support physicians when making effective treatment decisions,” said Fabio Piazzalunga, president and CEO of Menarini Silicon Biosystems. “As a company, we will continue to support research aimed at demonstrating the clinical utility of CTC and we maintain our commitment to improve patient management.”
Source: Read Full Article


