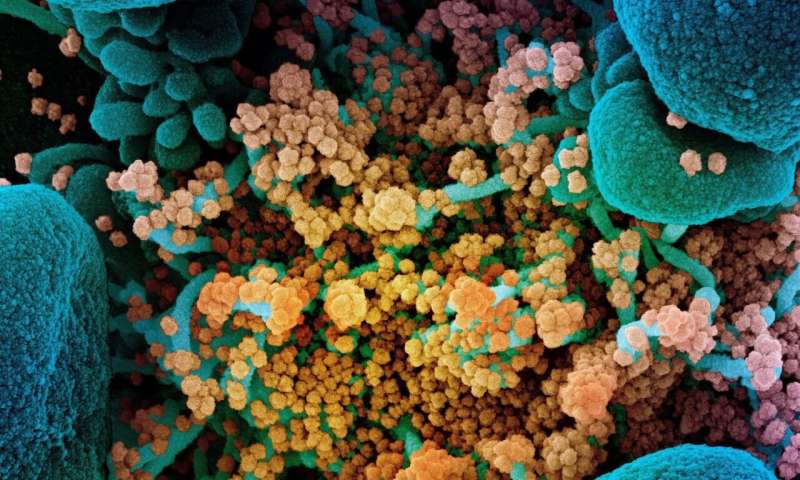
Study shows similar antibody response to key SARS-CoV-2 ‘spike’ protein in COVID-19
New research published in Diabetologia (the journal of the European Association for the Study of Diabetes) shows that antibody responses to SARS-CoV-2 are similar in COVID-19 patients with and without diabetes, and thus are unlikely to be responsible for the higher death rates in patients with diabetes.
Furthermore, they found that a particular antibody response related to the ‘spike’ protein of the SARS-CoV-2 virus is strongly associated with improved survival, boosting hopes that vaccines involving this same protein will have a high chance of being as effective in vulnerable patients with diabetes as they will be in the general population. The study also found that higher blood glucose levels were strongly associated with COVID-19 mortality in patients whether or not they had diabetes.
Patients with diabetes, especially type 2 diabetes, are over-represented in COVID-19 deaths and severe disease. In countries such as the UK, around 30% of people who have died with COVID-19 infection have also had diabetes, with similar numbers reported in other countries.
“Demonstrating the ability to mount an appropriate antibody response in the presence of abnormally high blood sugar (hyperglycaemia) is relevant to understand the mechanisms related to the observed worse clinical outcome of COVID-19 pneumonia in patients with diabetes and for the development of any future vaccination campaign to prevent SARS-CoV-2 infection,” explain the authors, who include Professor Lorenzo Piemonti, Director of the San Raffaele Diabetes Research Institute, IRCCS Hospital San Raffaele, Milan, Italy, and colleagues.
The authors analysed the presence of three types of antibody to COVID-19 in their study: immunoglobulin G (IgG), which is evidence of past infection; IgM, which indicates more recent or current infection, and IgA, which is involved in the mucosal immune response, for example in the nose and respiratory tract where the virus enters the body.
They analysed the IgG, IgM and IgA response against multiple antigens of SARS-CoV-2 in a cohort of 509 patients with documented diagnosis of COVID-19, prospectively followed at the IRCCS Hospital San Raffaele. These patients were all adults (aged 18 years or over) and admitted between 25 February and 19 April 2020. These patients had all signed consent forms to have blood samples taken and stored, in order to help with COVID-19 research efforts. The researchers analysed the patients’ clinical outcomes and antibody levels according to the presence of hyperglycaemia, including either diagnosed or undiagnosed diabetes, at the time of, or during, hospitalisation.
Among patients with confirmed COVID-19, 139 (27.3%) had diabetes: 90 (17.7%) had diabetes diagnosed prior to the hospital admission while 49 (9.6%) had diabetes diagnosed at the time of admission (newly diagnosed). Diabetes was associated with increased levels of inflammatory biomarkers and hypercoagulopathy (increased blood clotting), as well as leucocytosis (increased leukocytes, a type of white blood cell in the immune system) and neutrophilia (high levels of neutrophils, another type of white blood cell).
Diabetes was independently associated with 2.3 times increased risk of death, even after adjustment for age, sex and other relevant comorbidities. Furthermore, a strong association between higher glucose levels and risk of death was found, irrespective of diabetes diagnosis, with statistical modelling showing that each increase in blood sugar of 1.1 mmol/l resulted in a 14% increased risk of COVID-19 related death, regardless of whether the patient had diabetes. The range of blood sugar values in patients without diabetes was 4.1 to 6.6 mmol/l, while in those with diabetes the range was much greater, from 5.1 to 14.3 mmol/l.
The immune response in terms of the above antibodies against SARS-CoV-2 in patients with diabetes was present and almost identical, in both timing and antibody levels, to that of patients without diabetes, with only marginal differences. The response was also not influenced by blood glucose levels.
Of the measured antibody responses, positivity for IgG against the SARS-CoV-2 spike receptor-binding domain (RBD) (which the virus uses to enter human cells) was predictive of survival rate, both in the presence or absence of diabetes. Overall, the presence of these particular antibodies was associated with a 60% reduction in the death rate of patients with COVID-19, with a 63% reduction death risk in patients with diabetes, and a 57% reduction in those without. This is important, say the authors, because many SARS-CoV-2 vaccines currently in development are targeting this so-called ‘spike protein’ in the virus.
The authors say: “Patients with either diagnosed or undiagnosed diabetes are more likely to experience severe symptoms and death from COVID-19 pneumonia. Frailty, pre-existing comorbid conditions and a potential underlying immune system dysfunction could contribute to a poorer outcome.”
Source: Read Full Article


